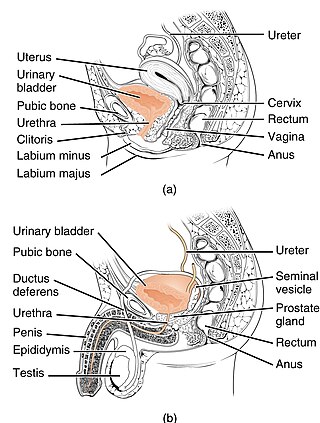
Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the urinary-tract system and the reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.
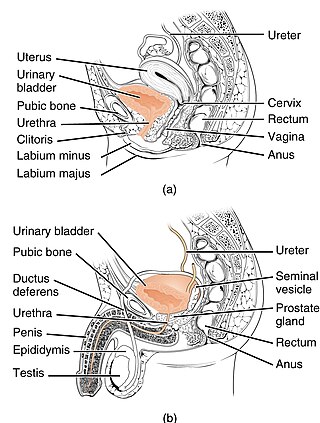
The urethra is a tube that connects the urinary bladder to the urinary meatus for the removal of urine from the body of both females and males. In human females and other primates, the urethra connects to the urinary meatus above the vagina, whereas in marsupials, the female's urethra empties into the urogenital sinus.
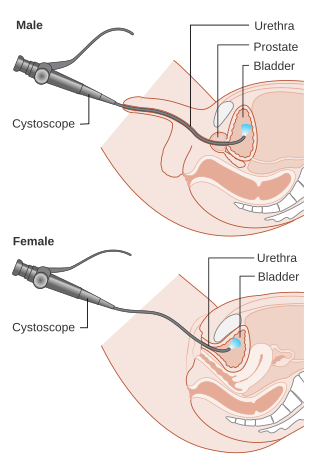
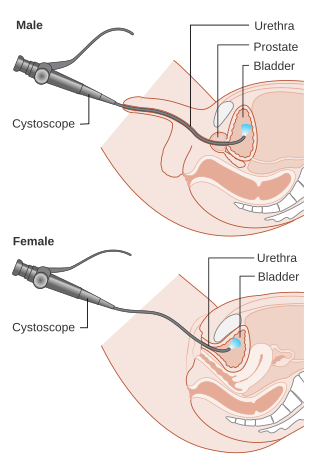
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.

In urinary catheterization, a latex, polyurethane, or silicone tube known as a urinary catheter is inserted into the bladder through the urethra to allow urine to drain from the bladder for collection. It may also be used to inject liquids used for treatment or diagnosis of bladder conditions. A clinician, often a nurse, usually performs the procedure, but self-catheterization is also possible. A catheter may be in place for long periods of time or removed after each use.

A urethral stricture is a narrowing of the urethra, the tube connected to the bladder that allows the passing of urine. The narrowing reduces the flow of urine and makes it more difficult or even painful to empty the bladder.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.

In urology, a Foley catheter is a brand name for one of many brands of urinary catheters (UC). Foleys and their namesakes are indwelling UC, often referred to as an IDCs or the alternative type being an in/out catheters. The foley UC was named after Frederic Foley, who produced the original design in 1929. The UC is a flexible tube if it is indwelling and stays put, or rigid if it is in/out, that a clinician, or the client themselves, often in the case of in/out UC, passes it through the urethra and into the bladder to drain urine.

A urostomy is a surgical procedure that creates a stoma for the urinary system. A urostomy is made to avail for urinary diversion in cases where drainage of urine through the bladder and urethra is not possible, e.g. after extensive surgery or in case of obstruction.
An Indiana pouch is a surgically-created urinary diversion used to create a way for the body to store and eliminate urine for patients who have had their urinary bladders removed as a result of bladder cancer, pelvic exenteration, bladder exstrophy or who are not continent due to a congenital, neurogenic bladder. This particular urinary diversion results in a continent reservoir that the patient must catheterize to empty urine. This concept and technique was developed by Drs. Mike Mitchell, Randall Rowland, and Richard Bihrle at Indiana University.
A urethrotomy is an operation which involves incision of the urethra, especially for relief of a stricture. It is most often performed in the outpatient setting, with the patient (usually) being discharged from the hospital or surgery center within six hours from the procedure's inception.

Posterior urethral valve (PUV) disorder is an obstructive developmental anomaly in the urethra and genitourinary system of male newborns. A posterior urethral valve is an obstructing membrane in the posterior male urethra as a result of abnormal in utero development. It is the most common cause of bladder outlet obstruction in male newborns. The disorder varies in degree, with mild cases presenting late due to milder symptoms. More severe cases can have renal and respiratory failure from lung underdevelopment as result of low amniotic fluid volumes, requiring intensive care and close monitoring. It occurs in about one in 8,000 babies.
In urology, voiding cystourethrography (VCUG) is a frequently performed technique for visualizing a person's urethra and urinary bladder while the person urinates (voids). It is used in the diagnosis of vesicoureteral reflux, among other disorders. The technique consists of catheterizing the person in order to fill the bladder with a radiocontrast agent, typically diatrizoic acid. Under fluoroscopy the radiologist watches the contrast enter the bladder and looks at the anatomy of the patient. If the contrast moves into the ureters and back into the kidneys, the radiologist makes the diagnosis of vesicoureteral reflux, and gives the degree of severity a score. The exam ends when the person voids while the radiologist is watching under fluoroscopy. Consumption of fluid promotes excretion of contrast media after the procedure. It is important to watch the contrast during voiding, because this is when the bladder has the most pressure, and it is most likely this is when reflux will occur. Despite this detailed description of the procedure, at least as of 2016 the technique had not been standardized across practices.

A ureteral stent, or ureteric stent, is a thin tube inserted into the ureter to prevent or treat obstruction of the urine flow from the kidney. The length of the stents used in adult patients varies between 24 and 30 cm. Additionally, stents come in differing diameters or gauges, to fit different size ureters. The stent is usually inserted with the aid of a cystoscope. One or both ends of the stent may be coiled to prevent it from moving out of place; this is called a JJ stent, double J stent or pig-tail stent.
Neurogenic bladder dysfunction, or neurogenic bladder, refers to urinary bladder problems due to disease or injury of the central nervous system or peripheral nerves involved in the control of urination. There are multiple types of neurogenic bladder depending on the underlying cause and the symptoms. Symptoms include overactive bladder, urinary urgency, frequency, incontinence or difficulty passing urine. A range of diseases or conditions can cause neurogenic bladder including spinal cord injury, multiple sclerosis, stroke, brain injury, spina bifida, peripheral nerve damage, Parkinson's disease, or other neurodegenerative diseases. Neurogenic bladder can be diagnosed through a history and physical as well as imaging and more specialized testing. Treatment depends on underlying disease as well as symptoms and can be managed with behavioral changes, medications, surgeries, or other procedures. The symptoms of neurogenic bladder, especially incontinence, can have a significant impact on quality of life.
Urethroplasty is the surgical repair of an injury or defect within the walls of the urethra. Trauma, iatrogenic injury and infections are the most common causes of urethral injury/defect requiring repair. Urethroplasty is regarded as the gold standard treatment for urethral strictures and offers better outcomes in terms of recurrence rates than dilatations and urethrotomies. It is probably the only useful modality of treatment for long and complex strictures though recurrence rates are higher for this difficult treatment group.

A retrograde urethrography is a routine radiologic procedure used to image the integrity of the urethra. Hence a retrograde urethrogram is essential for diagnosis of urethral injury, or urethral stricture.

Urethrostomy is a surgical procedure that creates a permanent opening in the urethra, commonly to remove obstructions to urine flow. The procedure is most often performed in male cats, where the opening is made in the perineum.
Bladder outlet obstruction occurs when urine is unable to flow from the kidneys through the ureters and out of the bladder through the urethra. Decreased flow of urine leads to swelling of the urinary tract, called hydronephrosis. This process of decreased flow of urine through the urinary tract can begin as early as during intrauterine life and it prevents normal development of fetal kidneys and fetal urine. Low levels of fetal urine leads to low amniotic fluid levels and incomplete lung maturation. Older children and adults can also experience bladder outlet obstruction; however, this process is usually reversible and isn't associated with as many poor outcomes as in infants with congenital bladder outlet obstruction.
Suprapubic aspiration is a procedure to take a urine sample. It involves putting a needle through the skin just above the pubic bone into the bladder. It is typically used as a method to collect urine in child less than 2 years of age who is not yet toilet trained in an effort to diagnose a urinary tract infection.
The genitourinary tract, or simply the urinary tract, consists of the kidneys, ureters, bladder, and the urethra. The kidney is the most frequently injured. Injuries to the kidney commonly occur after automobile or sports-related accidents. A blunt force is involved in 80-85% of injuries. Major decelerations can result in vascular injuries near the kidney's hilum. Gunshots and knife wounds and fractured ribs can result in penetrating injuries to the kidney.