Related Research Articles

Candidiasis is a fungal infection due to any species of the genus Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers, among other symptoms.

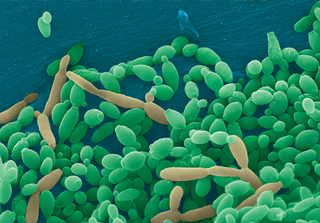
Staphylococcus aureus is a gram-positive spherically shaped bacterium, a member of the Bacillota, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive for catalase and nitrate reduction and is a facultative anaerobe that can grow without the need for oxygen. Although S. aureus usually acts as a commensal of the human microbiota, it can also become an opportunistic pathogen, being a common cause of skin infections including abscesses, respiratory infections such as sinusitis, and food poisoning. Pathogenic strains often promote infections by producing virulence factors such as potent protein toxins, and the expression of a cell-surface protein that binds and inactivates antibodies. S. aureus is one of the leading pathogens for deaths associated with antimicrobial resistance and the emergence of antibiotic-resistant strains, such as methicillin-resistant S. aureus (MRSA), is a worldwide problem in clinical medicine. Despite much research and development, no vaccine for S. aureus has been approved.

Lactobacillus is a genus of gram-positive, aerotolerant anaerobes or microaerophilic, rod-shaped, non-spore-forming bacteria. Until 2020, the genus Lactobacillus comprised over 260 phylogenetically, ecologically, and metabolically diverse species; a taxonomic revision of the genus assigned lactobacilli to 25 genera.

The human microbiome is the aggregate of all microbiota that reside on or within human tissues and biofluids along with the corresponding anatomical sites in which they reside, including the gastrointestinal tract, skin, mammary glands, seminal fluid, uterus, ovarian follicles, lung, saliva, oral mucosa, conjunctiva, and the biliary tract. Types of human microbiota include bacteria, archaea, fungi, protists, and viruses. Though micro-animals can also live on the human body, they are typically excluded from this definition. In the context of genomics, the term human microbiome is sometimes used to refer to the collective genomes of resident microorganisms; however, the term human metagenome has the same meaning.
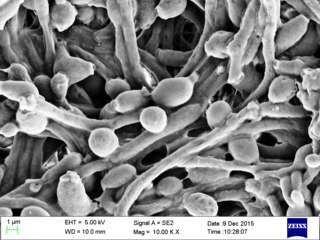
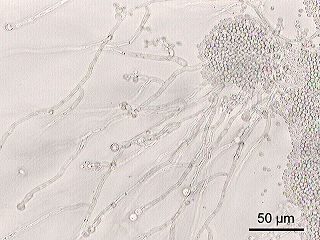
Candida albicans is an opportunistic pathogenic yeast that is a common member of the human gut flora. It can also survive outside the human body. It is detected in the gastrointestinal tract and mouth in 40–60% of healthy adults. It is usually a commensal organism, but it can become pathogenic in immunocompromised individuals under a variety of conditions. It is one of the few species of the genus Candida that cause the human infection candidiasis, which results from an overgrowth of the fungus. Candidiasis is, for example, often observed in HIV-infected patients. C. albicans is the most common fungal species isolated from biofilms either formed on (permanent) implanted medical devices or on human tissue. C. albicans, C. tropicalis, C. parapsilosis, and C. glabrata are together responsible for 50–90% of all cases of candidiasis in humans. A mortality rate of 40% has been reported for patients with systemic candidiasis due to C. albicans. By one estimate, invasive candidiasis contracted in a hospital causes 2,800 to 11,200 deaths yearly in the US. Nevertheless, these numbers may not truly reflect the true extent of damage this organism causes, given new studies indicating that C. albicans can cross the blood–brain barrier in mice.
Candida is a genus of yeasts. It is the most common cause of fungal infections worldwide and the largest genus of medically important yeasts.

Oral candidiasis (Acute pseudomembranous candidiasis), also known as oral thrush among other names, is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis (yeast/fungal infection) of Candida species on the mucous membranes of the mouth.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

An opportunistic infection is an infection caused by pathogens that take advantage of an opportunity not normally available. These opportunities can stem from a variety of sources, such as a weakened immune system, an altered microbiome, or breached integumentary barriers. Many of these pathogens do not necessarily cause disease in a healthy host that has a non-compromised immune system, and can, in some cases, act as commensals until the balance of the immune system is disrupted. Opportunistic infections can also be attributed to pathogens which cause mild illness in healthy individuals but lead to more serious illness when given the opportunity to take advantage of an immunocompromised host.

Fungemia is the presence of fungi or yeast in the blood. The most common type, also known as candidemia, candedemia, or systemic candidiasis, is caused by Candida species. Candidemia is also among the most common bloodstream infections of any kind. Infections by other fungi, including Saccharomyces, Aspergillus and Cryptococcus, are also called fungemia. It is most commonly seen in immunosuppressed or immunocompromised patients with severe neutropenia, cancer patients, or in patients with intravenous catheters. It has been suggested that otherwise immunocompetent patients taking infliximab may also be at a higher risk.
Candida parapsilosis is a fungal species of yeast that has become a significant cause of sepsis and of wound and tissue infections in immunocompromised people. Unlike Candida albicans and Candida tropicalis, C. parapsilosis is not an obligate human pathogen, having been isolated from nonhuman sources such as domestic animals, insects and soil. C. parapsilosis is also a normal human commensal and it is one of the fungi most frequently isolated from human hands. There are several risk factors that can contribute to C. parapsilosis colonization. Immunocompromised individuals and surgical patients, particularly those undergoing surgery of the gastrointestinal tract, are at high risk for infection with C. parapsilosis. There is currently no consensus on the treatment of invasive candidiasis caused by C. parapsilosis, although the therapeutic approach typically includes the removal of foreign bodies such as implanted prostheses and the administration of systemic antifungal therapy. Amphotericin B and Fluconazole are often used in the treatment of C. parapsilosis infection.
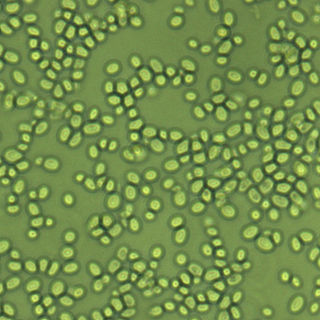
Nakaseomyces glabratus is a species of haploid yeast of the genus Nakaseomyces, previously known as Candida glabrata. Despite the fact that no sexual life cycle has been documented for this species, N. glabratus strains of both mating types are commonly found. N. glabrata is generally a commensal of human mucosal tissues, but in today's era of wider human immunodeficiency from various causes, N. glabratus is often the second or third most common cause of candidiasis as an opportunistic pathogen. Infections caused by N. glabratus can affect the urogenital tract or even cause systemic infections by entrance of the fungal cells in the bloodstream (Candidemia), especially prevalent in immunocompromised patients.
A skin infection is an infection of the skin in humans and other animals, that can also affect the associated soft tissues such as loose connective tissue and mucous membranes. They comprise a category of infections termed skin and skin structure infections (SSSIs), or skin and soft tissue infections (SSTIs), and acute bacterial SSSIs (ABSSSIs). They are distinguished from dermatitis, although skin infections can result in skin inflammation.
Pathogenic fungi are fungi that cause disease in humans or other organisms. Although fungi are eukaryotic, many pathogenic fungi are microorganisms. Approximately 300 fungi are known to be pathogenic to humans; their study is called "medical mycology". Fungal infections are estimated to kill more people than either tuberculosis or malaria—about two million people per year.
Oral ecology is the microbial ecology of the microorganisms found in mouths. Oral ecology, like all forms of ecology, involves the study of the living things found in oral cavities as well as their interactions with each other and with their environment. Oral ecology is frequently investigated from the perspective of oral disease prevention, often focusing on conditions such as dental caries, candidiasis ("thrush"), gingivitis, periodontal disease, and others. However, many of the interactions between the microbiota and oral environment protect from disease and support a healthy oral cavity. Interactions between microbes and their environment can result in the stabilization or destabilization of the oral microbiome, with destabilization believed to result in disease states. Destabilization of the microbiome can be influenced by several factors, including diet changes, drugs or immune system disorders.
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.

Hwp1 is a protein (glycoprotein) located on the surface of an opportunistic diploid fungus called Candida albicans.
Invasive candidiasis is an infection (candidiasis) that can be caused by various species of Candida yeast. Unlike Candida infections of the mouth and throat or vagina, invasive candidiasis is a serious, progressive, and potentially fatal infection that can affect the blood (fungemia), heart, brain, eyes, bones, and other parts of the body.
Candida tropicalis is a species of yeast in the genus Candida. It is a common pathogen in neutropenic hosts, in whom it may spread through the bloodstream to peripheral organs. For invasive disease, treatments include amphotericin B, echinocandins, or extended-spectrum triazole antifungals.
Carol Kumamoto is an American microbiologist who is Professor of Molecular Biology & Microbiology at Tufts University. She investigates the filamentous growth of Candida albicans, a fungal pathogen that causes several diseases. She is also interested in how C. albicans interacts with its host during colonisation and invasive diseases. She is a Fellow of the American Association for the Advancement of Science and the American Academy of Microbiology.
References
- ↑ "LIAS Glossary". Archived from the original on 11 December 2013. Retrieved 14 August 2013.
- ↑ Copetti, Marina V.; Iamanaka, Beatriz T.; Frisvad, Jens C.; Pereira, José L.; Taniwaki, Marta H. (December 2011). "Mycobiota of cocoa: From farm to chocolate". Food Microbiology. 28 (8): 1499–1504. doi: 10.1016/j.fm.2011.08.005 . PMID 21925035.
- 1 2 Mukherjee, Pranab K.; Sendid, Boualem; Hoarau, Gautier; Colombel, Jean-Frédéric; Poulain, Daniel; Ghannoum, Mahmoud A. (February 2015). "Mycobiota in gastrointestinal diseases". Nature Reviews. Gastroenterology & Hepatology. 12 (2): 77–87. doi:10.1038/nrgastro.2014.188. ISSN 1759-5053. PMID 25385227. S2CID 5370536.
- ↑ Kerawala, C; Newlands, C, eds. (2010). Oral and maxillofacial surgery. Oxford: Oxford University Press. pp. 446, 447. ISBN 978-0-19-920483-0.
- 1 2 3 Erdogan, Askin; Rao, Satish S. C. (April 2015). "Small Intestinal Fungal Overgrowth". Current Gastroenterology Reports. 17 (4). doi:10.1007/s11894-015-0436-2. S2CID 3098136.
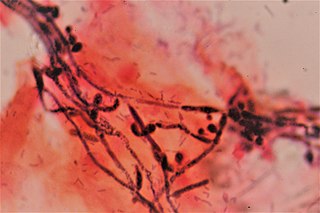
Small intestinal fungal overgrowth (SIFO) is characterized by the presence of excessive number of fungal organisms in the small intestine associated with gastrointestinal (GI) symptoms. Candidiasis is known to cause GI symptoms particularly in immunocompromised patients or those receiving steroids or antibiotics. However, only recently, there is emerging literature that an overgrowth of fungus in the small intestine of non-immunocompromised subjects may cause unexplained GI symptoms. Two recent studies showed that 26 % (24/94) and 25.3 % (38/150) of a series of patients with unexplained GI symptoms had SIFO. The most common symptoms observed in these patients were belching, bloating, indigestion, nausea, diarrhea, and gas. ... Fungal-bacterial interaction may act in different ways and may either be synergistic or antagonistic or symbiotic [29]. Some bacteria such as Lactobacillus species can interact and inhibit both the virulence and growth of Candida species in the gut by producing hydrogen peroxide [30]. Any damage to the mucosal barrier or disruption of GI microbiota with chemotherapy or antibiotic use, inflammatory processes, activation of immune molecules and disruption of epithelial repair may all cause fungal overgrowth [27].
- ↑ Peters, Brian M.; Jabra-Rizk, Mary Ann; Scheper, Mark A.; Leid, Jeff G.; Costerton, John William; Shirtliff, Mark E. (2010). "Microbial interactions and differential protein expression in Staphylococcus aureus–Candida albicans dual-species biofilms". FEMS Immunology & Medical Microbiology. 59 (3): 493–503. doi:10.1111/j.1574-695X.2010.00710.x. PMC 2936118 . PMID 20608978.
- ↑ Lin, Yi Jey; Alsad, Lina; Vogel, Fabio; Koppar, Shardul; Nevarez, Leslie; Auguste, Fabrice; Seymour, John; Syed, Aisha; Christoph, Kristina; Loomis, Joshua S. (2013). "Interactions between Candida albicans and Staphylococcus aureus within mixed species biofilms". BIOS. 84: 30–39. doi:10.1893/0005-3155-84.1.30. S2CID 96930404.
- ↑ Zago, Chaiene Evelin; Silva, Sónia; Sanitá, Paula Volpato; Barbugli, Paula Aboud; Dias, Carla Maria Improta; Lordello, Virgínia Barreto; Vergani, Carlos Eduardo (2015). "Dynamics of Biofilm Formation and the Interaction between Candida albicans and Methicillin-Susceptible (MSSA) and -Resistant Staphylococcus aureus (MRSA)". PLOS ONE. 10 (4): e0123206. Bibcode:2015PLoSO..1023206Z. doi: 10.1371/journal.pone.0123206 . PMC 4395328 . PMID 25875834.
- ↑ Tortora, Gerald J. (2010). Microbiology: An Introduction. San Francisco, CA: Pearson Benjamin Cummings. p. 758.
- 1 2 Calderone, A; Clancy, CJ, eds. (2012). Candida and Candidiasis (2nd ed.). ASM Press. ISBN 978-1-55581-539-4.
- ↑ Weinberger, M (2016-04-16). "Characteristics of candidaemia with Candida-albicans compared with non-albicans Candida species and predictors of mortality". J Hosp Infect. 61 (2): 146–54. doi:10.1016/j.jhin.2005.02.009. PMID 16009456.
- 1 2 Cui, Lijia; Morris, Alison; Ghedin, Elodie (2013). "The human mycobiome in health and disease". Genome Medicine. 5 (7): 63. doi: 10.1186/gm467 . PMC 3978422 . PMID 23899327.
- 1 2 Martins, Natália; Ferreira, Isabel C. F. R.; Barros, Lillian; Silva, Sónia; Henriques, Mariana (June 2014). "Candidiasis: Predisposing Factors, Prevention, Diagnosis and Alternative Treatment" (PDF). Mycopathologia. 177 (5–6): 223–240. doi:10.1007/s11046-014-9749-1. hdl: 10198/10147 . S2CID 795450. Archived (PDF) from the original on 2017-08-17. Retrieved 2019-09-19.
- 1 2 Wang, Z. K.; Yang, Y. S.; Stefka, A. T.; Sun, G.; Peng, L. H. (April 2014). "Review article: fungal microbiota and digestive diseases". Alimentary Pharmacology & Therapeutics. 39 (8): 751–766. doi: 10.1111/apt.12665 .
- ↑ Marcon, M J; Powell, D A (April 1992). "Human infections due to Malassezia spp". Clinical Microbiology Reviews. 5 (2): 101–119. doi:10.1128/CMR.5.2.101. PMC 358230 . PMID 1576583.
- ↑ Roth, R R; James, W D (October 1988). "Microbial Ecology of the Skin". Annual Review of Microbiology. 42 (1): 441–464. doi:10.1146/annurev.mi.42.100188.002301. PMID 3144238.
- ↑ Freedberg; et al., eds. (2003). Fitzpatrick's Dermatology in General Medicine (6th ed.). McGraw-Hill. p. 1187. ISBN 0-07-138067-1.