Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage."
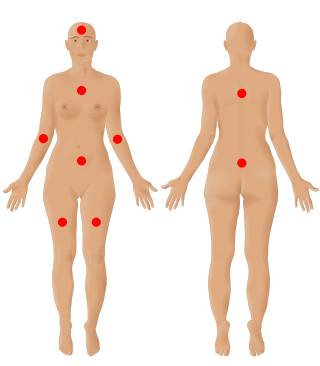
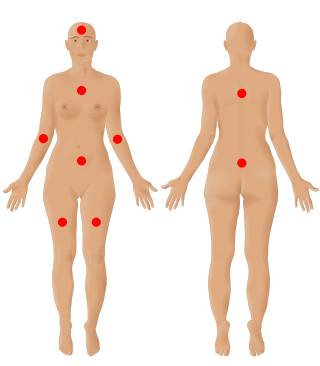
Fibromyalgia is a medical syndrome which commonly presents as chronic widespread pain, accompanied by fatigue, waking unrefreshed, and cognitive symptoms. Other symptoms include headaches, lower abdominal pain or cramps, and depression. People with fibromyalgia can also experience insomnia and a general hypersensitivity. The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors. Environmental factors may include psychological stress, trauma, and certain infections. Since the pain appears to result from processes in the central nervous system, the condition is referred to as a "central sensitization syndrome".

Itch is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.

Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

Hyperalgesia is an abnormally increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves and can cause hypersensitivity to stimulus. Prostaglandins E and F are largely responsible for sensitizing the nociceptors. Temporary increased sensitivity to pain also occurs as part of sickness behavior, the evolved response to infection.
Neuropathic pain is pain caused by a lesion or disease of the somatosensory nervous system. Neuropathic pain may be associated with abnormal sensations called dysesthesia or pain from normally non-painful stimuli (allodynia). It may have continuous and/or episodic (paroxysmal) components. The latter resemble stabbings or electric shocks. Common qualities include burning or coldness, "pins and needles" sensations, numbness and itching.

Referred pain, also called reflective pain, is pain perceived at a location other than the site of the painful stimulus. An example is the case of angina pectoris brought on by a myocardial infarction, where pain is often felt in the left side of neck, left shoulder, and back rather than in the thorax (chest), the site of the injury. The International Association for the Study of Pain has not officially defined the term; hence, several authors have defined it differently. Referred pain has been described since the late 1880s. Despite an increasing amount of literature on the subject, the biological mechanism of referred pain is unknown, although there are several hypotheses.
Sensitization is a non-associative learning process in which repeated administration of a stimulus results in the progressive amplification of a response. Sensitization often is characterized by an enhancement of response to a whole class of stimuli in addition to the one that is repeated. For example, repetition of a painful stimulus may make one more responsive to a loud noise.

Allodynia is a condition in which pain is caused by a stimulus that does not normally elicit pain. For example, sunburn can cause temporary allodynia, so that usually painless stimuli, such as wearing clothing or running cold or warm water over it, can be very painful. It is different from hyperalgesia, an exaggerated response from a normally painful stimulus. The term comes from Ancient Greek άλλος (állos) 'other', and οδύνη (odúnē) 'pain'.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.
Pain tolerance is the maximum level of pain that a person is able to tolerate. Pain tolerance is distinct from pain threshold. The perception of pain that goes in to pain tolerance has two major components. First is the biological component—the headache or skin prickling that activates pain receptors. Second is the brain’s perception of pain—how much focus is spent paying attention to or ignoring the pain. The brain’s perception of pain is a response to signals from pain receptors that sensed the pain in the first place.

Transient receptor potential cation channel subfamily M (melastatin) member 8 (TRPM8), also known as the cold and menthol receptor 1 (CMR1), is a protein that in humans is encoded by the TRPM8 gene. The TRPM8 channel is the primary molecular transducer of cold somatosensation in humans. In addition, mints can desensitize a region through the activation of TRPM8 receptors.

Nav1.8 is a sodium ion channel subtype that in humans is encoded by the SCN10A gene.
Psychogenic pain is physical pain that is caused, increased, or prolonged by mental, emotional, or behavioral factors, without evidence of physical injury or illness.

The wide dynamic range (WDR) neuron was first discovered by Mendell in 1966. Early studies of this neuron established what is known as the gate control theory of pain. The basic concept is that non-painful stimuli block the pathways for painful stimuli, inhibiting possible painful responses. This theory was supported by the fact that WDR neurons are responsible for responses to both painful and non-painful stimuli, and the idea that these neurons could not produce more than one of these responses simultaneously. WDR neurons respond to all types of somatosensory stimuli, make up the majority of the neurons found in the posterior grey column, and have the ability to produce long range responses including those responsible for pain and itch.

There is a scientific debate which questions whether crustaceans experience pain. It is a complex mental state, with a distinct perceptual quality but also associated with suffering, which is an emotional state. Because of this complexity, the presence of pain in an animal, or another human for that matter, cannot be determined unambiguously using observational methods, but the conclusion that animals experience pain is often inferred on the basis of likely presence of phenomenal consciousness which is deduced from comparative brain physiology as well as physical and behavioural reactions.
Diffuse noxious inhibitory controls (DNIC) or conditioned pain modulation (CPM) refers to an endogenous pain modulatory pathway which has often been described as "pain inhibits pain". It occurs when response from a painful stimulus is inhibited by another, often spatially distant, noxious stimulus.

Pain in cephalopods is a contentious issue. Pain is a complex mental state, with a distinct perceptual quality but also associated with suffering, which is an emotional state. Because of this complexity, the presence of pain in non-human animals, or another human for that matter, cannot be determined unambiguously using observational methods, but the conclusion that animals experience pain is often inferred on the basis of likely presence of phenomenal consciousness which is deduced from comparative brain physiology as well as physical and behavioural reactions.
Ocular neuropathic pain is a spectrum of disorders of ocular pain which are caused by damage or disease affecting the nerves. Ocular neuropathic pain is frequently associated with damaged or dysfunctional corneal nerves, but the condition can also be caused by peripheral or centralized sensitization. The condition shares some characteristics with somatic neuropathic pain in that it is similarly associated with abnormal sensations (dysesthesia) or pain from normally non-painful stimuli (allodynia), but until recent years has been poorly understood by the medical community, and frequently dismissed by ophthalmologists who were not trained to identify neuropathic pain as a source of unexplained eye pain beyond objective findings noted on slit-lamp examination.
Epigenetics of chronic pain is the study of how epigenetic modifications of genes affect the development and maintenance of chronic pain. Chromatin modifications have been found to affect neural function, such as synaptic plasticity and memory formation, which are important mechanisms of chronic pain. In 2019, 20% of adults dealt with chronic pain. Epigenetics can provide a new perspective on the biological mechanisms and potential treatments of chronic pain.