Related Research Articles

Schizophrenia is a mental disorder characterized by reoccurring episodes of psychosis that are correlated with a general misperception of reality. Other common signs include hallucinations, delusions, disorganized thinking, social withdrawal, and flat affect. Symptoms develop gradually and typically begin during young adulthood and are never resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months or one month. Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.
Anti-psychiatry, sometimes spelled antipsychiatry without the hyphen, is a movement based on the view that psychiatric treatment is often more damaging than helpful to patients, highlighting controversies about psychiatry. Objections include the reliability of psychiatric diagnosis, the questionable effectiveness and harm associated with psychiatric medications, the failure of psychiatry to demonstrate any disease treatment mechanism for psychiatric medication effects, and legal concerns about equal human rights and civil freedom being nullified by the presence of diagnosis. Historical critiques of psychiatry came to light after focus on the extreme harms associated with electroconvulsive therapy or insulin shock therapy. The term "anti-psychiatry" is in dispute and often used to dismiss all critics of psychiatry, many of whom agree that a specialized role of helper for people in emotional distress may at times be appropriate, and allow for individual choice around treatment decisions.
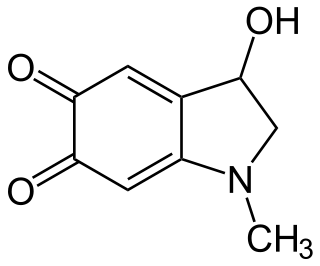
Adrenochrome is a chemical compound produced by the oxidation of adrenaline (epinephrine). It was the subject of limited research from the 1950s through to the 1970s as a potential cause of schizophrenia. While it has no current medical application, the semicarbazide derivative, carbazochrome, is a hemostatic medication.
Richard Bentall is a Professor of Clinical Psychology at the University of Sheffield in the UK.
Orthomolecular medicine is a form of alternative medicine that claims to maintain human health through nutritional supplementation. It is rejected by evidence-based medicine. The concept builds on the idea of an optimal nutritional environment in the body and suggests that diseases reflect deficiencies in this environment. Treatment for disease, according to this view, involves attempts to correct "imbalances or deficiencies based on individual biochemistry" by use of substances such as vitamins, minerals, amino acids, trace elements and fatty acids. The notions behind orthomolecular medicine are not supported by sound medical evidence, and the therapy is not effective for chronic disease prevention; even the validity of calling the orthomolecular approach a form of medicine has been questioned since the 1970s.
Historically, mental disorders have had three major explanations, namely, the supernatural, biological and psychological models. For much of recorded history, deviant behavior has been considered supernatural and a reflection of the battle between good and evil. When confronted with unexplainable, irrational behavior and by suffering and upheaval, people have perceived evil. In fact, in the Persian Empire from 550 to 330 B.C., all physical and mental disorders were considered the work of the devil. Physical causes of mental disorders have been sought in history. Hippocrates was important in this tradition as he identified syphilis as a disease and was, therefore, an early proponent of the idea that psychological disorders are biologically caused. This was a precursor to modern psycho-social treatment approaches to the causation of psychopathology, with the focus on psychological, social and cultural factors. Well known philosophers like Plato, Aristotle, etc., wrote about the importance of fantasies, dreams, and thus anticipated, to some extent, the fields of psychoanalytic thought and cognitive science that were later developed. They were also some of the first to advocate for humane and responsible care for individuals with psychological disturbances.

Ladislas Joseph Meduna was a Hungarian neuropathologist and neuropsychiatrist who initiated convulsive treatment, the repeated induction of grand mal seizures, as a treatment of psychosis. Observing the high concentration of glia in post-mortem brains of patients with epilepsy and a paucity in those with schizophrenia, he proposed that schizophrenia might be treated by inducing "epileptic" seizures. Thus, chemically induced seizures became the electroconvulsive therapy that is now in worldwide use.

Abram Hoffer was a Canadian biochemist, physician, and psychiatrist known for his "adrenochrome hypothesis" of schizoaffective disorders. According to Hoffer, megavitamin therapy and other nutritional interventions are potentially effective treatments for cancer and schizophrenia. Hoffer was also involved in studies of LSD as an experimental therapy for alcoholism and the discovery that high-dose niacin can be used to treat high cholesterol and other dyslipidemias. Hoffer's ideas about megavitamin therapy to treat mental illness are not accepted by the medical community.
Thought broadcasting is a type of delusional condition in which the affected person believes that others can hear their inner thoughts, despite a clear lack of evidence. The person may believe that either those nearby can perceive their thoughts or that they are being transmitted via mediums such as television, radio or the internet. Different people can experience thought broadcasting in different ways. Thought broadcasting is most commonly found among people who have a psychotic disorder, specifically schizophrenia.

Insulin shock therapy or insulin coma therapy was a form of psychiatric treatment in which patients were repeatedly injected with large doses of insulin in order to produce daily comas over several weeks. It was introduced in 1927 by Austrian-American psychiatrist Manfred Sakel and used extensively in the 1940s and 1950s, mainly for schizophrenia, before falling out of favour and being replaced by neuroleptic drugs in the 1960s.
Megavitamin therapy is the use of large doses of vitamins, often many times greater than the recommended dietary allowance (RDA) in the attempt to prevent or treat diseases. Megavitamin therapy is typically used in alternative medicine by practitioners who call their approach orthomolecular medicine. Vitamins are useful in preventing and treating illnesses specifically associated with dietary vitamin shortfalls, but the conclusions of medical research are that the broad claims of disease treatment by advocates of megavitamin therapy are unsubstantiated by the available evidence. It is generally accepted that doses of any vitamin greatly in excess of nutritional requirements will result either in toxicity or in the excess simply being metabolised; thus evidence in favour of vitamin supplementation supports only doses in the normal range. Critics have described some aspects of orthomolecular medicine as food faddism or even quackery. Research on nutrient supplementation in general suggests that some nutritional supplements might be beneficial, and that others might be harmful; several specific nutritional therapies are associated with an increased likelihood of the condition they are meant to prevent.
Irwin Stone (1907–1984) was an American biochemist, chemical engineer, and writer. He was the first to use ascorbic acid in the food processing industry as a preservative, and originated and published the hypothesis that humans require much larger amounts of Vitamin C for optimal health than is necessary to prevent scurvy.
The Journal of Orthomolecular Medicine was established in 1967 by Abram Hoffer. It publishes studies in nutritional and orthomolecular medicine. There is controversy surrounding the journal, as the validity of the field of orthomolecular medicine is not widely accepted by mainstream medicine. The journal is ranked in the bottom 10 percent of all journals about complementary and alternative medicine that are indexed in the bibliographic database Scopus.
Primary polydipsia and psychogenic polydipsia are forms of polydipsia characterised by excessive fluid intake in the absence of physiological stimuli to drink. Psychogenic polydipsia which is caused by psychiatric disorders, often schizophrenia, is often accompanied by the sensation of dry mouth. Some forms of polydipsia are explicitly non-psychogenic. Primary polydipsia is a diagnosis of exclusion.

The Soteria model is a milieu-therapeutic approach developed to treat acute schizophrenia, usually implemented in Soteria houses.
Carl Curt Pfeiffer was a physician and biochemist who researched schizophrenia, allergies and other diseases. He was Chair of the Pharmacology Department at Emory University and considered himself a founder of what two-time Nobel prize winner, [Pauling, PhD.], named orthomolecular psychiatry and published in the Journal Science. 1968 Apr 19;160(3825):265-71.
The management of schizophrenia usually involves many aspects including psychological, pharmacological, social, educational, and employment-related interventions directed to recovery, and reducing the impact of schizophrenia on quality of life, social functioning, and longevity.

Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, perceptions, and emotions.
The relationship between religion and schizophrenia is of particular interest to psychiatrists because of the similarities between religious experiences and psychotic episodes. Religious experiences often involve reports of auditory and/or visual phenomena, which sounds seemingly similar to those with schizophrenia who also commonly report hallucinations and delusions. These symptoms may resemble the events found within a religious experience. However, the people who report these religious visual and audio hallucinations also claim to have not perceived them with their five senses, rather, they conclude these hallucinations were an entirely internal process. This differs from schizophrenia, where the person is unaware that their own thoughts or inner feelings are not happening outside of them. They report hearing, seeing, smelling, feeling, or tasting something that deludes them to believe it is real. They are unable to distinguish between reality and hallucinations because they experience these hallucinations with their bodily senses that leads them to perceive these events as happening outside of their mind. In general, religion has been found to have "both a protective and a risk increasing effect" for schizophrenia.
The outcomes paradox is the observation that patients with schizophrenia in developing countries benefit much more from therapy than those in developed countries. This is surprising because the reverse holds for most diseases: "the richer and more developed the country, the better the patient outcome." The outcomes paradox came to light in the 1960s due to cross-cultural studies conducted by the World Health Organization on the outcome of severe mental disorders like schizophrenia. This paradox has become an axiom in international psychiatry since.
References
- ↑ Saul, AW; Jolliffe M; Hoffer A. "Bibliography of the Publications of Carl Pfeiffer, MD, PhD". doctoryourself.com. Retrieved 2007-04-19.
- ↑ Reiter, PJ (1927). "Behandlung von Dementia Praecox mit metallsalzen. Mangan. Z". Neur. 108: 464–80. doi:10.1007/bf02863975. as cited in Pfeiffer, C; LaMola, S (1983). "Zinc and Manganese in the Schizophrenias". Journal of Orthomolecular Psychiatry. 12 (3).
- ↑ Kay Lily E (1993). The molecular vision of life: Caltech, the Rockefeller Foundation, and the rise of the new biology. Oxford: Oxford University Press. ISBN 978-0-19-511143-9.
- 1 2 3 4 Edelman Eva (2001). Natural Healing for Schizophrenia: And Other Common Mental Disorders. Borage Books. ISBN 978-0-9650976-7-3.
- ↑ Barney, Paul (1998). Doctor's guide to natural medicine. Pleasant Grove, Utah: Woodland. ISBN 978-1-885670-84-7.
- ↑ Pauling L (1968). "Orthomolecular psychiatry. Varying the concentrations of substances normally present in the human body may control mental disease" (PDF). Science . 160 (3825): 265–71. Bibcode:1968Sci...160..265P. doi:10.1126/science.160.3825.265. PMID 5641253. S2CID 20153555.
- ↑ Pauling, Linus; Hawkins, D (1973). Orthomolecular psychiatry: treatment of schizophrenia. San Francisco: W.H. Freeman. p. 697. ISBN 978-0-7167-0898-8.
- 1 2 Menolascino FJ, Donaldson JY, Gallagher TF, Golden CJ, Wilson JE (1988). "Orthomolecular therapy: its history and applicability to psychiatric disorders". Child Psychiatry Hum Dev. 18 (3): 133–50. doi:10.1007/BF00709727. PMID 2898324. S2CID 38354755.
- ↑ Pauling L, Wyatt RJ, Klein DF, Lipton MA (1974). "On the orthomolecular environment of the mind: orthomolecular theory". American Journal of Psychiatry. 131 (11): 1251–67. doi:10.1176/ajp.131.11.1251 (inactive 31 January 2024). PMID 4608217.
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link) - ↑ Lerner, V (2005-08-31). "Treatment of acute schizophrenia with vitamin therapy". Clinicaltrials.gov. Retrieved 2008-01-15.
- ↑ Hoffer, Abram. "The History of the Journal of Orthomolecular Medicine". J Orthomol Med. Archived from the original on 2011-05-20. Retrieved 2011-06-18.
- 1 2 Barrett MD, Stephen (2000-07-12). "Orthomolecular Therapy". Quackwatch . Retrieved 2008-01-02.
- ↑ Laperchia, P. (1987). "Behavioral disorders, learning disabilities and megavitamin therapy". Adolescence. 22 (87): 729–738. PMID 2963502.
- ↑ "Pyroluria". nutritional-healing.com. Archived from the original on 2008-02-26. Retrieved 2008-02-17.
- ↑ Jackson James A; Riordan Hugh D; Neathery Sharon; Riordan Neil H (1997). "Urinary pyrrole in health and disease" (PDF). The Journal of Orthomolecular Medicine. 12 (2nd Quarter): 96–8. Retrieved 2008-02-17.
- 1 2 Skertic, Mark (April 21, 2002). "For some, a question of balancing nutrients". SunTimes.com. Available at the internet archive. Retrieved on 2008-02-17
- ↑ Holman, Paul (July 1995). "Pyridoxine - Vitamin B-6" (PDF). Journal of Australian College of Nutritional & Environmental Medicine. 14 (1): 5–16. Archived from the original (PDF) on 2007-05-08. Retrieved 2007-04-19.
- ↑ Cruz, R; Vogel, WH (1978). "Pyroluria: a poor marker in chronic schizophrenia". The American Journal of Psychiatry. 135 (10): 1239–40. doi:10.1176/ajp.135.10.1239. PMID 696910.
- ↑ Gendler, PL; Duhan, HA; Rapoport, H (1978). "Hemopyrrole and kryptopyrrole are absent from the urine of schizophrenics and normal persons". Clinical Chemistry. 24 (2): 230–3. doi:10.1093/clinchem/24.2.230. PMID 627053.
- ↑ Jacobson, SJ; Rapoport, H; Ellman, GL (1975). "The nonoccurrence of hemo- and kryptopyrrole in urine of schizophrenics". Biological Psychiatry. 10 (1): 91–3. PMID 1120177.
- ↑ Gorchein, A (1980). "Urine concentration of 3-ethyl-5-hydroxy-4,5-dimethyl-delta 3-pyrrolin-2-one ('mauve factor') is not causally related to schizophrenia or to acute intermittent porphyria". Clinical Science. 58 (6): 469–76. doi:10.1042/cs0580469. PMID 7428279.
- ↑ Vaughan, K.; McConaghy, N. (1999). "Megavitamin and dietary treatment in schizophrenia: a randomised, controlled trial". The Australian and New Zealand Journal of Psychiatry. 33 (1): 84–88. doi:10.1046/j.1440-1614.1999.00527.x. PMID 10197889. S2CID 38857700.
- ↑ National Library for Health (2005-10-05). "What is pyroluria, is it an accepted clinical entity and what are the treatment?". Archived from the original on 2007-02-11.
- ↑ Pfeiffer Carl C, et al. (July 1971). "Blood histamine levels, basophil counts, and trace metals in the schizophrenias". Psychopharmacol Bull. 7 (3): 37. PMID 5117854.
- ↑ Pfeiffer Carl C; Smyrl, EG; Iliev, V (July 1972). "Extreme basophil counts and blood histamine levels in schizophrenic outpatients as compared to normals". Res Commun Chem Pathol Pharmacol. 4 (1): 51–9. PMID 4671910.
- ↑ Pfeiffer Carl C (1988). Nutrition and Mental Illness: An Orthomolecular Approach to Balancing Body Chemistry. Healing Arts Press. ISBN 978-0-89281-226-4.
- ↑ Pfeiffer, Carl C (1987). Nutrition and Mental Illness: An Orthomolecular Approach to Balancing Body Chemistry. Healing Art Press. ISBN 978-0-89281-226-4.
- ↑ Miller M (1996). "Diet and psychological health". Altern Ther Health Med. 2 (5): 40–8. PMID 8795935.
- ↑ Bennett, Forrest C (November 1983). "Vitamin and mineral supplementation in Down's syndrome". Pediatrics. 72 (5): 707–713. doi:10.1542/peds.72.5.707. PMID 6226926. S2CID 1888682.
- ↑ Lipton M, et al. (1973). Task force report on megavitamin and orthomolecular Therapy in psychiatry. Washington DC: American Psychiatric Association.; as cited in Barrett MD, Stephen (2000-07-12). "Orthomolecular Therapy". Quackwatch . Retrieved 2008-01-02.