Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender. The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals. It is also known as sex reassignment surgery, gender confirmation surgery, and several other names.

Metoidioplasty, metaoidioplasty, or metaidoioplasty is a female-to-male gender-affirming surgery.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.
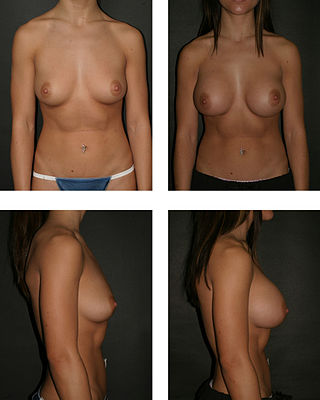
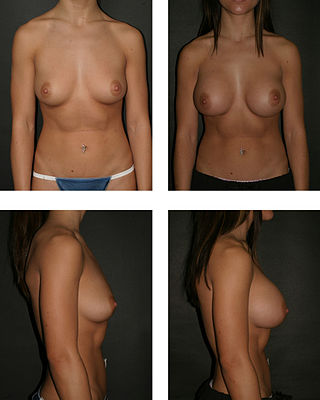
Breast augmentation and augmentation mammoplasty is a cosmetic surgery technique using breast-implants and fat-graft mammoplasty techniques to increase the size, change the shape, and alter the texture of the breasts. Although in some cases augementation mammoplasty is applied to correct congenital defects of the breasts and the chest wall in other cases it is used purely as a cosmetic surgery, primary breast augmentation changes the aesthetics – of size, shape, and texture – of healthy breasts.
Vaginoplasty is any surgical procedure that results in the construction or reconstruction of the vagina. It is a type of genitoplasty. Pelvic organ prolapse is often treated with one or more surgeries to repair the vagina. Sometimes a vaginoplasty is needed following the treatment or removal of malignant growths or abscesses to restore a normal vaginal structure and function. Surgery to the vagina is done to correct congenital defects to the vagina, urethra and rectum. It may correct protrusion of the urinary bladder into the vagina (cystocele) and protrusion of the rectum (rectocele) into the vagina. Often, a vaginoplasty is performed to repair the vagina and its attached structures due to trauma or injury.
Genital reconstructive surgery may refer to:

Scrotoplasty, also known as oscheoplasty, is a type of surgery to create or repair the scrotum. The history of male genital plastic surgery is rooted in many cultures and dates back to ancient times. However, scientific research for male genital plastic surgery such as scrotoplasty began to develop in the early 1900s. The development of testicular implants began in 1940 made from materials outside of what is used today. Today, testicular implants are created from saline or gel filled silicone rubber. There are a variety of reasons why scrotoplasty is done. Some transgender men and intersex or non-binary people who were assigned female at birth may choose to have this surgery to create a scrotum, as part of their transition. Other reasons for this procedure include addressing issues with the scrotum due to birth defects, aging, or medical conditions such as infection. For newborn males with penoscrotal defects such as webbed penis, a condition in which the penile shaft is attached to the scrotum, scrotoplasty can be performed to restore normal appearance and function. For older male adults, the scrotum may extend with age. Scrotoplasty or scrotal lift can be performed to remove the loose, excess skin. Scrotoplasty can also be performed for males who undergo infection, necrosis, traumatic injury of the scrotum.

Gluteoplasty denotes the plastic surgery and the liposuction procedures for the correction of congenital, traumatic, and acquired defects/deformities of the buttocks and the anatomy of the gluteal region; and for the aesthetic enhancement of the contour of the buttocks.

Vaginectomy is a surgery to remove all or part of the vagina. It is one form of treatment for individuals with vaginal cancer or rectal cancer that is used to remove tissue with cancerous cells. It can also be used in gender-affirming surgery. Some people born with a vagina who identify as trans men or as nonbinary may choose vaginectomy in conjunction with other surgeries to make the clitoris more penis-like (metoidioplasty), construct of a full-size penis (phalloplasty), or create a relatively smooth, featureless genital area.
Mastopexy is the plastic surgery mammoplasty procedure for raising sagging breasts upon the chest of the woman, by changing and modifying the size, contour, and elevation of the breasts. In a breast-lift surgery to re-establish an aesthetically proportionate bust for the woman, the critical corrective consideration is the tissue viability of the nipple-areola complex (NAC), to ensure the functional sensitivity of the breasts for lactation and breast-feeding.
Penis transplantation is a surgical transplant procedure in which a penis is transplanted to a patient. The penis may be an allograft from a human donor, or it may be grown artificially, though the latter has not yet been transplanted onto a human.

A penile implant is an implanted device intended for the treatment of erectile dysfunction, Peyronie's disease, ischemic priapism, deformity and any traumatic injury of the penis, and for phalloplasty or metoidioplasty, including in gender-affirming surgery. Men also opt for penile implants for aesthetic purposes. Men's satisfaction and sexual function is influenced by discomfort over genital size which leads to seek surgical and non-surgical solutions for penis alteration. Although there are many distinct types of implants, most fall into one of two categories: malleable and inflatable transplants.
Urethroplasty is the surgical repair of an injury or defect within the walls of the urethra. Trauma, iatrogenic injury and infections are the most common causes of urethral injury/defect requiring repair. Urethroplasty is regarded as the gold standard treatment for urethral strictures and offers better outcomes in terms of recurrence rates than dilatations and urethrotomies. It is probably the only useful modality of treatment for long and complex strictures though recurrence rates are higher for this difficult treatment group.

Gary J. Alter is an American plastic surgeon. His specialties include sex reassignment surgery, genital reconstruction surgery and facial feminization surgery. He appeared in two episodes of the reality television series, Dr. 90210. PRNewswire reported on June 5, 2015 that Dr. Gary J. Alter performed the body work plastic surgery on Caitlyn Jenner. He has a practice in Beverly Hills, CA.

Buried penis, also called hidden penis or retractile penis, is a congenital or acquired condition in which the penis is partially or completely hidden below the surface of the skin. A buried penis can lead to urinary difficulties, poor hygiene, infection, and inhibition of normal sexual function.

Webbed penis also known as buried or concealed penis is an acquired or congenital condition in which the scrotal skin extends onto the ventral penile shaft. The penile shaft is buried in the scrotum or tethered to the scrotal midline by a fold or web of skin. The urethra and erectile bodies are usually normal. Webbed penis is usually asymptomatic, but the cosmetic appearance is often unacceptable. This condition may be corrected by surgical techniques.

Miroslav L Djordjevic is a Serbian surgeon specializing in sex reassignment surgery, and an assistant professor of urology at the School of Medicine, University of Belgrade, Serbia.

Zephyr Surgical Implants (ZSI) is a Swiss-based medical device manufacturer that produces and distributes artificial urinary sphincters and penile implants worldwide. ZSI products are used in the management of moderate-to-severe urinary incontinence in men, erectile dysfunction, Peyronie's disease, penis enlargement, and female-to-male gender reassignment surgery.
Penile implants may be employed to treat erectile dysfunction or urinary troubles after a spinal cord injury.