Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose below 70 mg/dL (3.9 mmol/L), symptoms associated with hypoglycemia, and resolution of symptoms when blood sugar returns to normal. Hypoglycemia may result in headache, tiredness, clumsiness, trouble talking, confusion, fast heart rate, sweating, shakiness, nervousness, hunger, loss of consciousness, seizures, or death. Symptoms typically come on quickly.
The following is a glossary of diabetes which explains terms connected with diabetes.

The glucose tolerance test is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, insulin resistance, impaired beta cell function, and sometimes reactive hypoglycemia and acromegaly, or rarer disorders of carbohydrate metabolism. In the most commonly performed version of the test, an oral glucose tolerance test (OGTT), a standard dose of glucose is ingested by mouth and blood levels are checked two hours later. Many variations of the GTT have been devised over the years for various purposes, with different standard doses of glucose, different routes of administration, different intervals and durations of sampling, and various substances measured in addition to blood glucose.

Hyperglycemia is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/l (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/l (~250–300 mg/dL). A subject with a consistent range between ~5.6 and ~7 mmol/l is considered slightly hyperglycemic, and above 7 mmol/l is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.

Diabetic coma is a life-threatening but reversible form of coma found in people with diabetes mellitus.

Glycaemia, also known as blood sugar level, blood sugar concentration, or blood glucose level is the measure of glucose concentrated in the blood of humans or other animals. Approximately 4 grams of glucose, a simple sugar, is present in the blood of a 70 kg (154 lb) human at all times. The body tightly regulates blood glucose levels as a part of metabolic homeostasis. Glucose is stored in skeletal muscle and liver cells in the form of glycogen; in fasting individuals, blood glucose is maintained at a constant level at the expense of glycogen stores in the liver and skeletal muscle.

Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes generally results in few symptoms; however, it does increase the risk of pre-eclampsia, depression, and requiring a Caesarean section. Babies born to mothers with poorly treated gestational diabetes are at increased risk of being too large, having low blood sugar after birth, and jaundice. If untreated, it can also result in a stillbirth. Long term, children are at higher risk of being overweight and developing type 2 diabetes.

Dumping syndrome occurs when food, especially sugar, moves too quickly from the stomach to the duodenum—the first part of the small intestine—in the upper gastrointestinal (GI) tract. This condition is also called rapid gastric emptying. It is mostly associated with conditions following gastric or esophageal surgery, though it can also arise secondary to diabetes or to the use of certain medications; it is caused by an absent or insufficiently functioning pyloric sphincter, the valve between the stomach and the duodenum.

A glucose meter, also referred to as a "glucometer", is a medical device for determining the approximate concentration of glucose in the blood. It can also be a strip of glucose paper dipped into a substance and measured to the glucose chart. It is a key element of home blood glucose monitoring (HBGM) by people with diabetes mellitus or hypoglycemia. A small drop of blood, obtained by pricking the skin with a lancet, is placed on a disposable test strip that the meter reads and uses to calculate the blood glucose level. The meter then displays the level in units of mg/dL or mmol/L.

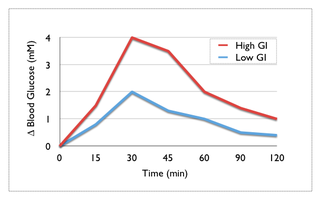
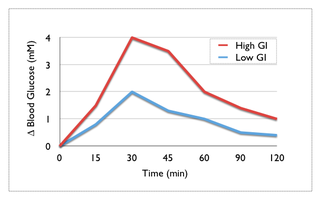
Reactive hypoglycemia, postprandial hypoglycemia, or sugar crash is a term describing recurrent episodes of symptomatic hypoglycemia occurring within four hours after a high carbohydrate meal in people with and without diabetes. The term is not necessarily a diagnosis since it requires an evaluation to determine the cause of the hypoglycemia.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate normal glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentration of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.
Many types of glucose tests exist and they can be used to estimate blood sugar levels at a given time or, over a longer period of time, to obtain average levels or to see how fast body is able to normalize changed glucose levels. Eating food for example leads to elevated blood sugar levels. In healthy people these levels quickly return to normal via increased cellular glucose uptake which is primarily mediated by increase in blood insulin levels.

For pregnant women with diabetes, some particular challenges exist for both mother and child. If the pregnant woman has diabetes as a pre-existing disorder, it can cause early labor, birth defects, and larger than average infants. Therefore, experts advise diabetics to maintain blood sugar level close to normal range about 3 months before planning for pregnancy.
Hyperosmolar hyperglycemic state (HHS) is a complication of diabetes mellitus in which high blood sugar results in high osmolarity without significant ketoacidosis. Symptoms include signs of dehydration, weakness, leg cramps, vision problems, and an altered level of consciousness. Onset is typically over days to weeks. Complications may include seizures, disseminated intravascular coagulopathy, mesenteric artery occlusion, or rhabdomyolysis.
Rabson–Mendenhall syndrome is a rare autosomal recessive disorder characterized by severe insulin resistance. The disorder is caused by mutations in the insulin receptor gene. Symptoms include growth abnormalities of the head, face and nails, along with the development of acanthosis nigricans. Treatment involves controlling blood glucose levels by using insulin and incorporating a strategically planned, controlled diet. Also, direct actions against other symptoms may be taken This syndrome usually affects children and has a prognosis of 1–2 years.
Chronic Somogyi rebound is a contested explanation of phenomena of elevated blood sugars in the morning. Also called the Somogyi effect and posthypoglycemic hyperglycemia, it is a rebounding high blood sugar that is a response to low blood sugar. When managing the blood glucose level with insulin injections, this effect is counter-intuitive to people who experience high blood sugar in the morning as a result of an overabundance of insulin at night.
A postprandial glucose (PPG) test is a blood glucose test that determines the amount of glucose, in the plasma after a meal. The diagnosis is typically restricted to postprandial hyperglycemia due to lack of strong evidence of co-relation with a diagnosis of diabetes.

1,5-Anhydroglucitol, also known as 1,5-AG, is a naturally occurring monosaccharide found in nearly all foods. Blood concentrations of 1,5-anhydroglucitol decrease during times of hyperglycemia above 180 mg/dL, and return to normal levels after approximately 2 weeks in the absence of hyperglycemia. As a result, it can be used for people with either type-1 or type-2 diabetes mellitus to identify glycemic variability or a history of high blood glucose even if current glycemic measurements such as hemoglobin A1c (HbA1c) and blood glucose monitoring have near normal values. Despite this possible use and its approval by the FDA, 1,5-AG tests are rarely ordered. There is some data suggesting that 1,5-AG values are useful to fill the gap and offer complementary information to HbA1c and fructosamine tests.
Neonatal hypoglycemia occurs when the neonate's blood glucose level is less than the newborn's body requirements for factors such as cellular energy and metabolism. There is inconsistency internationally for diagnostic thresholds. In the US, hypoglycemia is when the blood glucose level is below 30 mg/dl within the first 24 hours of life and below 45 mg/dl thereafter. In the UK, however, lower and more variable thresholds are used. The neonate's gestational age, birth weight, metabolic needs, and wellness state of the newborn has a substantial impact on the neonates blood glucose level. There are known risk factors that can be both maternal and neonatal. This is a treatable condition. Its treatment depends on the cause of the hypoglycemia. Though it is treatable, it can be fatal if gone undetected. Hypoglycemia is the most common metabolic problem in newborns.