Related Research Articles
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

Health informatics is the field of science and engineering that aims at developing methods and technologies for the acquisition, processing, and study of patient data, which can come from different sources and modalities, such as electronic health records, diagnostic test results, medical scans. The health domain provides an extremely wide variety of problems that can be tackled using computational techniques.

The Health Insurance Portability and Accountability Act of 1996 is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It modernized the flow of healthcare information, stipulates how personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and addressed some limitations on healthcare insurance coverage. It generally prohibits healthcare providers and healthcare businesses, called covered entities, from disclosing protected information to anyone other than a patient and the patient's authorized representatives without their consent. With limited exceptions, it does not restrict patients from receiving information about themselves. It does not prohibit patients from voluntarily sharing their health information however they choose, nor does it require confidentiality where a patient discloses medical information to family members, friends, or other individuals not a part of a covered entity.

The terms medical record, health record and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. A medical record includes a variety of types of "notes" entered over time by healthcare professionals, recording observations and administration of drugs and therapies, orders for the administration of drugs and therapies, test results, X-rays, reports, etc. The maintenance of complete and accurate medical records is a requirement of health care providers and is generally enforced as a licensing or certification prerequisite.
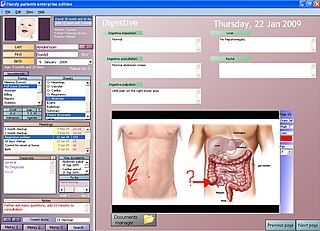
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.

A medical guideline is a document with the aim of guiding decisions and criteria regarding diagnosis, management, and treatment in specific areas of healthcare. Such documents have been in use for thousands of years during the entire history of medicine. However, in contrast to previous approaches, which were often based on tradition or authority, modern medical guidelines are based on an examination of current evidence within the paradigm of evidence-based medicine. They usually include summarized consensus statements on best practice in healthcare. A healthcare provider is obliged to know the medical guidelines of his or her profession, and has to decide whether to follow the recommendations of a guideline for an individual treatment.
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions and contains data entered by clinicians to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or from a smartphone.
Public health surveillance is, according to the World Health Organization (WHO), "the continuous, systematic collection, analysis and interpretation of health-related data needed for the planning, implementation, and evaluation of public health practice." Public health surveillance may be used to track emerging health-related issues at an early stage and find active solutions in a timely manner. Surveillance systems are generally called upon to provide information regarding when and where health problems are occurring and who is affected.
Utilization management (UM) or utilization review is the use of managed care techniques such as prior authorization that allow payers, particularly health insurance companies, to manage the cost of health care benefits by assessing its appropriateness before it is provided using evidence-based criteria or guidelines.
A Patient Safety Organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection and analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery
Evidence-based nursing (EBN) is an approach to making quality decisions and providing nursing care based upon personal clinical expertise in combination with the most current, relevant research available on the topic. This approach is using evidence-based practice (EBP) as a foundation. EBN implements the most up to date methods of providing care, which have been proven through appraisal of high quality studies and statistically significant research findings. The goal of EBN is to improve the health and safety of patients while also providing care in a cost-effective manner to improve the outcomes for both the patient and the healthcare system. EBN is a process founded on the collection, interpretation, appraisal, and integration of valid, clinically significant, and applicable research. The evidence used to change practice or make a clinical decision can be separated into seven levels of evidence that differ in type of study and level of quality. To properly implement EBN, the knowledge of the nurse, the patient's preferences, and multiple studies of evidence must all be collaborated and utilized in order to produce an appropriate solution to the task at hand. These skills are taught in modern nursing education and also as a part of professional training.

Medical diagnosis is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information required for diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes the posthumous diagnosis is considered a kind of medical diagnosis.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
Field triage is the process by which emergency medical services providers decide on the destination for the injured subject.
Online patient education, also known as online patient engagement, is a method of providing medical information and education to patients using learning management systems delivered through the Internet. It is a type of computer-based instruction and includes web seminars, downloadable materials, interactive learning courses, and audio/visual presentations. Generally, online patient education is supplemented with in-person consultations tailored to each individual.
Surgical scheduling software is computer software related to scheduling of tasks for a sequence of surgical cases in one surgery theatre and with one surgery staff using an operational model, a computer and a network. Another vital part of the surgery scheduling process is the communication between the Facility and the Vendor.
An automated dispensing cabinet (ADC) is a computerized medicine cabinet for hospitals and healthcare settings. ADCs allow medications to be stored and dispensed near the point of care while controlling and tracking drug distribution. They also are called unit-based cabinets (UBCs), automated dispensing devices (ADDs), automated distribution cabinets or automated dispensing machines (ADMs).
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.
A medical device hijack is a type of cyber attack. The weakness they target are the medical devices of a hospital. This was covered extensively in the press in 2015 and in 2016.
References
- 1 2 3 Coiera, E. (2003). Guide to Health Informatics. Great Britain: Hodder Education.
- ↑ Vissers, M.; Biert, J.; van der Liden, C.; Hasman, A. (1996). "Effects of a supportive protocol processing system (ProtoVIEW) on clinical behaviour of residents in the Accident and Emergency department". Computer Methods and Programs in Biomedicine. 49 (2): 177–184. doi:10.1016/0169-2607(95)01714-3. PMID 8735024.