Dengue fever is a mosquito-borne tropical disease caused by the dengue virus. Symptoms typically begin three to fourteen days after infection. These may include a high fever, headache, vomiting, muscle and joint pains, and a characteristic skin itching and skin rash. Recovery generally takes two to seven days. In a small proportion of cases, the disease develops into a more severe dengue hemorrhagic fever, resulting in bleeding, low levels of blood platelets and blood plasma leakage, or into dengue shock syndrome, where dangerously low blood pressure occurs.

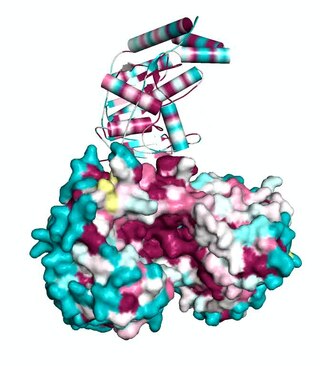
The enzyme-linked immunosorbent assay (ELISA) is a commonly used analytical biochemistry assay, first described by Eva Engvall and Peter Perlmann in 1971. The assay uses a solid-phase type of enzyme immunoassay (EIA) to detect the presence of a ligand in a liquid sample using antibodies directed against the protein to be measured. ELISA has been used as a diagnostic tool in medicine, plant pathology, and biotechnology, as well as a quality control check in various industries.

HIV tests are used to detect the presence of the human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS), in serum, saliva, or urine. Such tests may detect antibodies, antigens, or RNA.
A biosensor is an analytical device, used for the detection of a chemical substance, that combines a biological component with a physicochemical detector. The sensitive biological element, e.g. tissue, microorganisms, organelles, cell receptors, enzymes, antibodies, nucleic acids, etc., is a biologically derived material or biomimetic component that interacts with, binds with, or recognizes the analyte under study. The biologically sensitive elements can also be created by biological engineering. The transducer or the detector element, which transforms one signal into another one, works in a physicochemical way: optical, piezoelectric, electrochemical, electrochemiluminescence etc., resulting from the interaction of the analyte with the biological element, to easily measure and quantify. The biosensor reader device connects with the associated electronics or signal processors that are primarily responsible for the display of the results in a user-friendly way. This sometimes accounts for the most expensive part of the sensor device, however it is possible to generate a user friendly display that includes transducer and sensitive element. The readers are usually custom-designed and manufactured to suit the different working principles of biosensors.
Overdiagnosis is the diagnosis of disease that will never cause symptoms or death during a patient's ordinarily expected lifetime and thus presents no practical threat regardless of being pathologic. Overdiagnosis is a side effect of screening for early forms of disease. Although screening saves lives in some cases, in others it may turn people into patients unnecessarily and may lead to treatments that do no good and perhaps do harm. Given the tremendous variability that is normal in biology, it is inherent that the more one screens, the more incidental findings will generally be found. For a large percentage of them, the most appropriate medical response is to recognize them as something that does not require intervention; but determining which action a particular finding warrants can be very difficult, whether because the differential diagnosis is uncertain or because the risk ratio is uncertain.
Point-of-care testing (POCT), also called near-patient testing or bedside testing, is defined as medical diagnostic testing at or near the point of care—that is, at the time and place of patient care. This contrasts with the historical pattern in which testing was wholly or mostly confined to the medical laboratory, which entailed sending off specimens away from the point of care and then waiting hours or days to learn the results, during which time care must continue without the desired information.
Malaria antigen detection tests are a group of commercially available rapid diagnostic tests of the rapid antigen test type that allow quick diagnosis of malaria by people who are not otherwise skilled in traditional laboratory techniques for diagnosing malaria or in situations where such equipment is not available. There are currently over 20 such tests commercially available. The first malaria antigen suitable as target for such a test was a soluble glycolytic enzyme Glutamate dehydrogenase. None of the rapid tests are currently as sensitive as a thick blood film, nor as cheap. A major drawback in the use of all current dipstick methods is that the result is essentially qualitative. In many endemic areas of tropical Africa, however, the quantitative assessment of parasitaemia is important, as a large percentage of the population will test positive in any qualitative assay.
Loop-mediated isothermal amplification (LAMP) is a single-tube technique for the amplification of DNA and a low-cost alternative to detect certain diseases. Reverse transcription loop-mediated isothermal amplification (RT-LAMP) combines LAMP with a reverse transcription step to allow the detection of RNA.

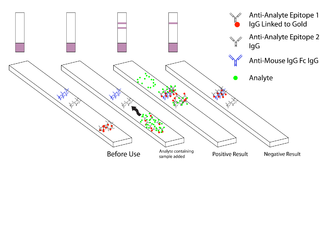
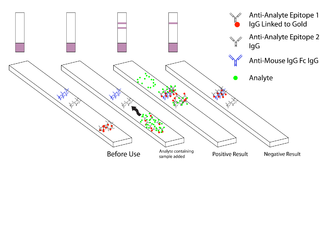
A lateral flow test (LFT), is an assay also known as a lateral flow device (LFD), lateral flow immunochromatographic assay, or rapid test. It is a simple device intended to detect the presence of a target substance in a liquid sample without the need for specialized and costly equipment. LFTs are widely used in medical diagnostics in the home, at the point of care, and in the laboratory. For instance, the home pregnancy test is an LFT that detects a specific hormone. These tests are simple and economical and generally show results in around five to thirty minutes. Many lab-based applications increase the sensitivity of simple LFTs by employing additional dedicated equipment. Because the target substance is often a biological antigen, many lateral flow tests are rapid antigen tests (RAT or ART).
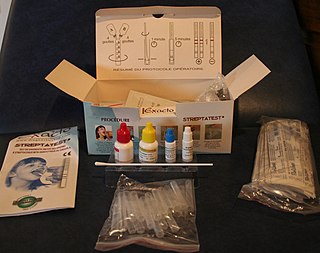
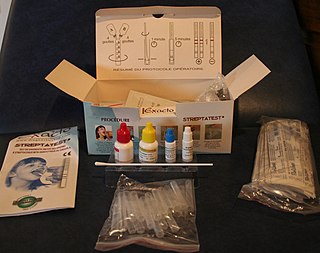
The rapid strep test (RST) is a rapid antigen detection test (RADT) that is widely used in clinics to assist in the diagnosis of bacterial pharyngitis caused by group A streptococci (GAS), sometimes termed strep throat. There are currently several types of rapid strep test in use, each employing a distinct technology. However, they all work by detecting the presence of GAS in the throat of a person by responding to GAS-specific antigens on a throat swab.

FIND is a global health non-profit based in Geneva, Switzerland. FIND functions as a product development partnership, engaging in active collaboration with over 150 partners to facilitate the development, evaluation, and implementation of diagnostic tests for poverty-related diseases. The organisation's Geneva headquarters are in Campus Biotech. Country offices are located in New Delhi, India; Cape Town, South Africa; and Hanoi, Viet Nam.
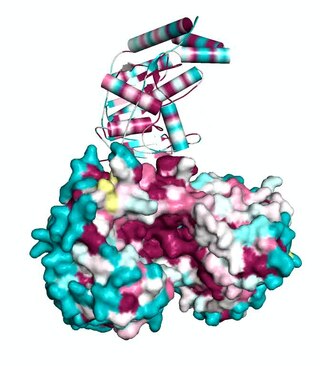
NS1 antigen test is a test for dengue, introduced in 2006. It allows rapid detection on the first day of fever, before antibodies appear some 5 or more days later. It has been adopted for use in some 40 nations. The method of detection is through enzyme-linked immunosorbent assay. India has introduced in 2010 the NS1 test costing 1,600 rupees at a private hospital in Mumbai.
The mainstay of malaria diagnosis has been the microscopic examination of blood, utilizing blood films. Although blood is the sample most frequently used to make a diagnosis, both saliva and urine have been investigated as alternative, less invasive specimens. More recently, modern techniques utilizing antigen tests or polymerase chain reaction have been discovered, though these are not widely implemented in malaria endemic regions. Areas that cannot afford laboratory diagnostic tests often use only a history of subjective fever as the indication to treat for malaria.
Flow-through tests or immunoconcentration assays are a type of diagnostic assay that allows users to test for the presence of a biomarker, usually a specific antibody, in a sample such as blood. They are a type of point of care test, a test designed to be used by a healthcare provider at patient contact. Point of care tests often allow for rapid detection of a specific biomarker without specialized lab equipment and training; this aids in diagnosis and allows therapeutic action to be initiated more quickly. Flow-through tests began development in the early 1980s and were the first type of immunostrip to be developed, although lateral flow tests have subsequently become the dominant immunostrip point of care device.
QuidelOrtho Corporation is a major American manufacturer of diagnostic healthcare products that are sold worldwide.
A rapid antigen test (RAT), sometimes called a rapid antigen detection test (RADT), antigen rapid test (ART), or loosely just a rapid test, is a rapid diagnostic test suitable for point-of-care testing that directly detects the presence or absence of an antigen. Such tests are a type of lateral flow test that detect antigens, distinguishing them from other medical tests that detect antibodies or nucleic acid, of either laboratory or point-of-care types. Rapid tests generally give a result in 5 to 30 minutes, require minimal training or infrastructure, and have significant cost advantages. Rapid antigen tests for the detection of SARS-CoV-2, the virus that causes COVID-19, have been commonly used during the COVID-19 pandemic.

Multiplexed point-of-care testing (xPOCT) is a more complex form of point-of-care testing (POCT), or bedside testing. Point-of-care testing is designed to provide diagnostic tests at or near the time and place that the patient is admitted. POCT uses the concentrations of analytes to provide the user with information on the physiological state of the patient. An analyte is a substance, chemical or biological, that is being analyzed using a certain instrument. While point-of-care testing is the quantification of one analyte from one in vitro sample, multiplexed point-of-care testing is the simultaneous on-site quantification of various analytes from a single sample.
Sosuga pararubulavirus is a species of Paramyxovirus which is transmissible to humans. The Egyptian fruit bat is thought to be a natural reservoir species for the virus.

COVID-19 testing involves analyzing samples to assess the current or past presence of SARS-CoV-2. The two main types of tests detect either the presence of the virus or antibodies produced in response to infection. Molecular tests for viral presence through its molecular components are used to diagnose individual cases and to allow public health authorities to trace and contain outbreaks. Antibody tests instead show whether someone once had the disease. They are less useful for diagnosing current infections because antibodies may not develop for weeks after infection. It is used to assess disease prevalence, which aids the estimation of the infection fatality rate.

COVID-19 rapid antigen tests or RATs, also frequently called COVID-19 lateral flow tests or LFTs, are rapid antigen tests used to detect SARS-CoV-2 infection (COVID-19). They are quick to implement with minimal training, cost a fraction of other forms of COVID-19 testing, and give users a result within 5–30 minutes. RATs have been used in several countries as part of mass testing or population-wide screening approaches. Many RATs can be used for self-testing, in which an individual "collects their own specimen… and interpret[s] their test result themselves".
Medical laboratory test.