Cardiac arrest, also known as sudden cardiac arrest, is when the heart suddenly and unexpectedly stops beating. As a result blood will not be pumped around the body in normal circulation, consciousness will be rapidly lost, and breathing will be abnormal or absent. Without immediate intervention such as cardiopulmonary resuscitation (CPR), and possibly defibrillation, death will occur within minutes.

Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation, or mouth to mouth in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest. It is recommended for those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.

Cardioversion is a medical procedure by which an abnormally fast heart rate (tachycardia) or other cardiac arrhythmia is converted to a normal rhythm using electricity or drugs. Synchronized electrical cardioversion uses a therapeutic dose of electric current to the heart at a specific moment in the cardiac cycle, restoring the activity of the electrical conduction system of the heart. Pharmacologic cardioversion, also called chemical cardioversion, uses antiarrhythmia medication instead of an electrical shock.

Advanced cardiac life support, advanced cardiovascular life support (ACLS) refers to a set of clinical guidelines for the urgent and emergent treatment of life-threatening cardiovascular conditions that will cause or have caused cardiac arrest, using advanced medical procedures, medications, and techniques. ACLS expands on Basic Life Support (BLS) by adding recommendations on additional medication and advanced procedure use to the CPR guidelines that are fundamental and efficacious in BLS. ACLS is practiced by advanced medical providers including physicians, some nurses and paramedics; these providers are usually required to hold certifications in ACLS care.

Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). A defibrillator delivers a dose of electric current to the heart. Although not fully understood, this process depolarizes a large amount of the heart muscle, ending the arrhythmia. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm. A heart which is in asystole (flatline) cannot be restarted by a defibrillator; it would be treated only by cardiopulmonary resuscitation (CPR) and medication, and then by cardioversion or defibrillation if it converts into a shockable rhythm.

Ventricular fibrillation is an abnormal heart rhythm in which the ventricles of the heart quiver. It is due to disorganized electrical activity. Ventricular fibrillation results in cardiac arrest with loss of consciousness and no pulse. This is followed by sudden cardiac death in the absence of treatment. Ventricular fibrillation is initially found in about 10% of people with cardiac arrest.

Asystole is the absence of ventricular contractions in the context of a lethal heart arrhythmia. Asystole is the most serious form of cardiac arrest and is usually irreversible. Also referred to as cardiac flatline, asystole is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
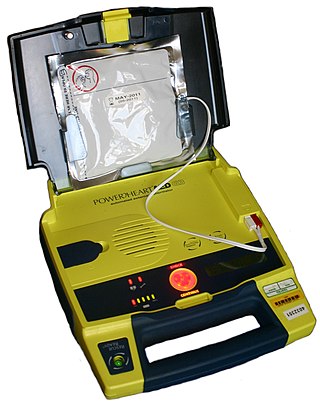
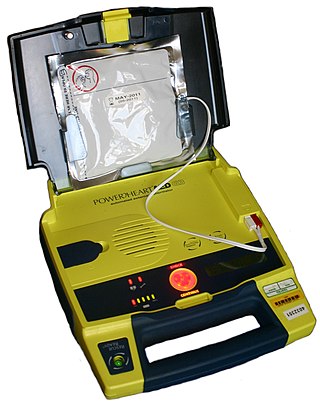
An automated external defibrillator or automatic electronic defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.

Ventricular tachycardia is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.
The Seattle & King County Emergency Medical Services System is a fire-based two-tier response system providing prehospital basic and advanced life support services.
Precordial thump is a medical procedure used in the treatment of ventricular fibrillation or pulseless ventricular tachycardia under certain conditions. The procedure has a very low success rate, but may be used in those with witnessed, monitored onset of one of the "shockable" cardiac rhythms if a defibrillator is not immediately available. It should not delay cardiopulmonary resuscitation (CPR) and defibrillation, nor should it be used in those with unwitnessed out-of-hospital cardiac arrest.

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.

A coronary care unit (CCU) or cardiac intensive care unit (CICU) is a hospital ward specialized in the care of patients with heart attacks, unstable angina, cardiac dysrhythmia and various other cardiac conditions that require continuous monitoring and treatment.

The AutoPulse is an automated, portable, battery-powered cardiopulmonary resuscitation device created by Revivant and subsequently purchased and currently manufactured by ZOLL Medical Corporation. It is a chest compression device composed of a constricting band and half backboard that is intended to be used as an adjunct to CPR during advanced cardiac life support by professional health care providers. The AutoPulse uses a distributing band to deliver the chest compressions. In literature it is also known as LDB-CPR.

Transcutaneous pacing (TCP), also called external pacing, is a temporary means of pacing a patient's heart during a medical emergency. It should not be confused with defibrillation using a manual or automatic defibrillator, though some newer defibrillators can do both, and pads and an electrical stimulus to the heart are used in transcutaneous pacing and defibrillation. Transcutaneous pacing is accomplished by delivering pulses of electric current through the patient's chest, which stimulates the heart to contract.
The chain of survival refers to a series of actions that, properly executed, reduce the mortality associated with sudden cardiac arrest. Like any chain, the chain of survival is only as strong as its weakest link. The six interdependent links in the chain of survival are early recognition of sudden cardiac arrest and access to emergency medical care, early CPR, early defibrillation, early advanced cardiac life support, and physical and emotional recovery. The first three links in the chain can be performed by lay bystanders, while the second three links are designated to medical professionals. Currently, between 70 and 90% of cardiac arrest patients die before they reach the hospital. However, a cardiac arrest does not have to be lethal if bystanders can take the right steps immediately.
The history of cardiopulmonary resuscitation (CPR) can be traced as far back as the literary works of ancient Egypt. However, it was not until the 18th century that credible reports of cardiopulmonary resuscitation began to appear in the medical literature.
A wearable cardioverter defibrillator (WCD) is a non-invasive, external device for patients at risk of sudden cardiac arrest (SCA). It allows physicians time to assess their patient's arrhythmic risk and see if their ejection fraction improves before determining the next steps in patient care. It is a leased device. A summary of the device, its technology and indications was published in 2017 and reviewed by the EHRA Scientific Documents Committee.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.
Return of spontaneous circulation (ROSC) is the resumption of a sustained heart rhythm that perfuses the body after cardiac arrest. It is commonly associated with significant respiratory effort. Signs of return of spontaneous circulation include breathing, coughing, or movement and a palpable pulse or a measurable blood pressure. Someone is considered to have sustained return of spontaneous circulation when circulation persists and cardiopulmonary resuscitation has ceased for at least 20 consecutive minutes.