Assistive technology (AT) is a term for assistive, adaptive, and rehabilitative devices for people with disabilities and the elderly. Disabled people often have difficulty performing activities of daily living (ADLs) independently, or even with assistance. ADLs are self-care activities that include toileting, mobility (ambulation), eating, bathing, dressing, grooming, and personal device care. Assistive technology can ameliorate the effects of disabilities that limit the ability to perform ADLs. Assistive technology promotes greater independence by enabling people to perform tasks they were formerly unable to accomplish, or had great difficulty accomplishing, by providing enhancements to, or changing methods of interacting with, the technology needed to accomplish such tasks. For example, wheelchairs provide independent mobility for those who cannot walk, while assistive eating devices can enable people who cannot feed themselves to do so. Due to assistive technology, disabled people have an opportunity of a more positive and easygoing lifestyle, with an increase in "social participation", "security and control", and a greater chance to "reduce institutional costs without significantly increasing household expenses." In schools, assistive technology can be critical in allowing students with disabilities to access the general education curriculum. Students who experience challenges writing or keyboarding, for example, can use voice recognition software instead. Assistive technologies assist people who are recovering from strokes and people who have sustained injuries that affect their daily tasks.
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.

A tremor is an involuntary, somewhat rhythmic, muscle contraction and relaxation involving oscillations or twitching movements of one or more body parts. It is the most common of all involuntary movements and can affect the hands, arms, eyes, face, head, vocal folds, trunk, and legs. Most tremors occur in the hands. In some people, a tremor is a symptom of another neurological disorder.

Apraxia is a motor disorder caused by damage to the brain, which causes difficulty with motor planning to perform tasks or movements. The nature of the damage determines the disorder's severity, and the absence of sensory loss or paralysis helps to explain the level of difficulty. Children may be born with apraxia; its cause is unknown, and symptoms are usually noticed in the early stages of development. Apraxia occurring later in life, known as acquired apraxia, is typically caused by traumatic brain injury, stroke, dementia, Alzheimer's disease, brain tumor, or other neurodegenerative disorders. The multiple types of apraxia are categorized by the specific ability and/or body part affected.

In medicine, a prosthesis, or a prosthetic implant, is an artificial device that replaces a missing body part, which may be lost through trauma, disease, or a condition present at birth. Prostheses are intended to restore the normal functions of the missing body part. Amputee rehabilitation is primarily coordinated by a physiatrist as part of an inter-disciplinary team consisting of physiatrists, prosthetists, nurses, physical therapists, and occupational therapists. Prostheses can be created by hand or with computer-aided design (CAD), a software interface that helps creators design and analyze the creation with computer-generated 2-D and 3-D graphics as well as analysis and optimization tools.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
The primary goals of stroke management are to reduce brain injury and promote maximum patient recovery. Rapid detection and appropriate emergency medical care are essential for optimizing health outcomes. When available, patients are admitted to an acute stroke unit for treatment. These units specialize in providing medical and surgical care aimed at stabilizing the patient's medical status. Standardized assessments are also performed to aid in the development of an appropriate care plan. Current research suggests that stroke units may be effective in reducing in-hospital fatality rates and the length of hospital stays.
The Bobath concept is an approach to neurological rehabilitation that is applied in patient assessment and treatment. The goal of applying the Bobath concept is to promote motor learning for efficient motor control in various environments, thereby improving participation and function. This is done through specific patient handling skills to guide patients through the initiation and completing of intended tasks. This approach to neurological rehabilitation is multidisciplinary, primarily involving physiotherapists, occupational therapists, and speech and language therapists. In the United States, the Bobath concept is also known as 'neuro-developmental treatment' (NDT).

The Hybrid Assistive Limb is a powered exoskeleton suit developed by Japan's Tsukuba University and the robotics company Cyberdyne. It is designed to support and expand the physical capabilities of its users, particularly people with physical disabilities. There are two primary versions of the system: HAL 3, which only provides leg function, and HAL 5, which is a full-body exoskeleton for the arms, legs, and torso.
Hypertonia is a term sometimes used synonymously with spasticity and rigidity in the literature surrounding damage to the central nervous system, namely upper motor neuron lesions. Impaired ability of damaged motor neurons to regulate descending pathways gives rise to disordered spinal reflexes, increased excitability of muscle spindles, and decreased synaptic inhibition. These consequences result in abnormally increased muscle tone of symptomatic muscles. Some authors suggest that the current definition for spasticity, the velocity-dependent over-activity of the stretch reflex, is not sufficient as it fails to take into account patients exhibiting increased muscle tone in the absence of stretch reflex over-activity. They instead suggest that "reversible hypertonia" is more appropriate and represents a treatable condition that is responsive to various therapy modalities like drug or physical therapy.
The goal of the LOPES project is to design and implement a gait rehabilitation robot for treadmill training. The target group consists of people who have had a stroke and have impaired motor control. The main goals of LOPES are:

Telerehabilitation (or e-rehabilitation is the delivery of rehabilitation services over telecommunication networks and the internet. Telerehabilitation allows patients to interact with providers remotely and can be used both to assess patients and to deliver therapy. Fields of medicine that utilize telerehabilitation include: physical therapy, occupational therapy, speech-language pathology, audiology, and psychology. Therapy sessions can be individual or community-based. Types of therapy available include motor training exercises, speech therapy, virtual reality, robotic therapy, goal setting, and group exercise.
Constraint-induced movement therapy is a form of rehabilitation therapy that improves upper extremity function in stroke and other central nervous system damage patients by increasing the use of their affected upper limb. Due to its high duration of treatment, the therapy has been found to frequently be infeasible when attempts have been made to apply it to clinical situations, and both patients and treating clinicians have reported poor compliance and concerns with patient safety. In the United States, the high duration of the therapy has also made the therapy not able to get reimbursed in most clinical environments.

Over time, the approach to cerebral palsy management has shifted away from narrow attempts to fix individual physical problems – such as spasticity in a particular limb – to making such treatments part of a larger goal of maximizing the person's independence and community engagement. Much of childhood therapy is aimed at improving gait and walking. Approximately 60% of people with CP are able to walk independently or with aids at adulthood. However, the evidence base for the effectiveness of intervention programs reflecting the philosophy of independence has not yet caught up: effective interventions for body structures and functions have a strong evidence base, but evidence is lacking for effective interventions targeted toward participation, environment, or personal factors. There is also no good evidence to show that an intervention that is effective at the body-specific level will result in an improvement at the activity level, or vice versa. Although such cross-over benefit might happen, not enough high-quality studies have been done to demonstrate it.

A powered exoskeleton is a mobile machine that is wearable over all or part of the human body, providing ergonomic structural support and powered by a system of electric motors, pneumatics, levers, hydraulics or a combination of cybernetic technologies, while allowing for sufficient limb movement with increased strength and endurance. The exoskeleton is designed to provide better mechanical load tolerance, and its control system aims to sense and synchronize with the user's intended motion and relay the signal to motors which manage the gears. The exoskeleton also protects the user's shoulder, waist, back and thigh against overload, and stabilizes movements when lifting and holding heavy items.

Ekso Bionics Holdings Inc. is a company that develops and manufactures powered exoskeleton bionic devices that can be strapped on as wearable robots to enhance the strength, mobility, and endurance of industrial workers and people experiencing paralysis and mobility issues after a brain injury, stroke, multiple sclerosis (MS) or spinal cord injury. They enable individuals with any amount of lower extremity weakness, including those who are paralyzed, to stand up and walk.
When treating a person with a spinal cord injury, repairing the damage created by injury is the ultimate goal. By using a variety of treatments, greater improvements are achieved, and, therefore, treatment should not be limited to one method. Furthermore, increasing activity will increase his/her chances of recovery.
Neuromechanics of orthoses refers to how the human body interacts with orthoses. Millions of people in the U.S. suffer from stroke, multiple sclerosis, postpolio, spinal cord injuries, or various other ailments that benefit from the use of orthoses. Insofar as active orthoses and powered exoskeletons are concerned, the technology to build these devices is improving rapidly, but little research has been done on the human side of these human-machine interfaces.
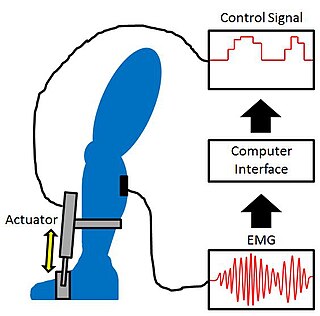
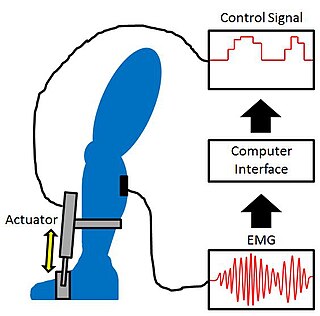
Proportional myoelectric control can be used to activate robotic lower limb exoskeletons. A proportional myoelectric control system utilizes a microcontroller or computer that inputs electromyography (EMG) signals from sensors on the leg muscle(s) and then activates the corresponding joint actuator(s) proportionally to the EMG signal.
Video game rehabilitation is a process of using common video game consoles and methodology to target and improve physical and mental weaknesses through therapeutic processes. Video games are becoming an integral part of occupational therapy practice in acute, rehabilitation, and community settings. The design for video games in rehabilitation is focused on a number of fundamental principles, such as reward, goals, challenge, and meaningful play. 'Meaningful play' emerges from the relationship between player action and system outcome, apparent to the player through, visual, physical and aural feedback. Platforms that feature motion control, notably the Nintendo Wii, Microsoft's Xbox Kinect, Sony's Eye Toy, and virtual reality have all been effective in this field of research. Methodologies have been applied to all age groups, from toddlers to the elderly. It has been used in a variety of cases ranging from stroke rehabilitation, cerebral palsy and other neurological impairments, to tendinitis and multiple sclerosis. Researchers have promoted such technology based on the personalization of gaming systems to patients, allowing for further engagement and interaction. Additionally, gaming consoles have the ability to capture real-time data and provide instant feedback to the patients using the systems. Currently, several researchers have performed case studies to demonstrate the benefits of this technology. Repeat trials and experiments have shown that outcomes are easily replicated among various groups worldwide. Additionally, the outcomes have increased interest in the field, growing experiments beyond simple case studies to experiments with a larger participant base.