Related Research Articles

The pleural cavity, pleural space, or interpleural space, is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication between the membranes, and also to create a pressure gradient.

A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung. Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.01 millilitre per kilogram weight per hour, and is cleared by lymphatic absorption leaving behind only 5–15 millilitres of fluid, which helps to maintain a functional vacuum between the parietal and visceral pleurae. Excess fluid within the pleural space can impair inspiration by upsetting the functional vacuum and hydrostatically increasing the resistance against lung expansion, resulting in a fully or partially collapsed lung.
Radiology (X-rays) is used in the diagnosis of tuberculosis. Abnormalities on chest radiographs may be suggestive of, but are never diagnostic of TB, but can be used to rule out pulmonary TB.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

Bronchiolitis obliterans (BO), also known as obliterative bronchiolitis, constrictive bronchiolitis and popcorn lung, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation. Symptoms include a dry cough, shortness of breath, wheezing and feeling tired. These symptoms generally get worse over weeks to months. It is not related to cryptogenic organizing pneumonia, previously known as bronchiolitis obliterans organizing pneumonia.
Mixed connective tissue disease commonly abbreviated as MCTD, is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP) together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.
Caplan's syndrome is a combination of rheumatoid arthritis (RA) and pneumoconiosis that manifests as intrapulmonary nodules, which appear homogenous and well-defined on chest X-ray.

Idiopathic pulmonary fibrosis (IPF) is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic scarring lung disease characterized by a progressive and irreversible decline in lung function. The tissue in the lungs becomes thick and stiff, which affects the tissue that surrounds the air sacs in the lungs. Symptoms typically include gradual onset of shortness of breath and a dry cough. Other changes may include feeling tired, and abnormally large and dome shaped finger and toenails. Complications may include pulmonary hypertension, heart failure, pneumonia or pulmonary embolism.

Usual interstitial pneumonia (UIP) is a form of lung disease characterized by progressive scarring of both lungs. The scarring (fibrosis) involves the pulmonary interstitium. UIP is thus classified as a form of interstitial lung disease.

High-resolution computed tomography (HRCT) is a type of computed tomography (CT) with specific techniques to enhance image resolution. It is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing the lung parenchyma. This article deals with high-resolution computed tomography of the lungs or HRCT Chest.

A rheumatoid nodule is a lump of tissue, or an area of swelling, that appear on the exterior of the skin usually around the olecranon or the interphalangeal joints, but can appear in other areas. There are four different types of rheumatoid nodules: subcutaneous rheumatoid nodules, cardiac nodules, pulmonary nodules, and central nervous systems nodules. These nodules occur almost exclusively in association with rheumatoid arthritis. Very rarely do rheumatoid nodules occur as rheumatoid nodulosis in the absence of rheumatoid arthritis. Rheumatoid nodules can also appear in other areas of the body other than the skin. Less commonly they occur in the lining of the lung or other internal organs. The occurrence of nodules in the lung of miners exposed to silica dust was known as Caplan’s syndrome. Rarely, the nodules occur at diverse sites on body.

Anti-citrullinated protein antibodies (ACPAs) are autoantibodies that are directed against peptides and proteins that are citrullinated. They are present in the majority of patients with rheumatoid arthritis. Clinically, cyclic citrullinated peptides (CCP) are frequently used to detect these antibodies in patient serum or plasma.

A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less than three millimetres. There may also be multiple nodules.

Respiratory bronchiolitis is a lung disease associated with tobacco smoking. In pathology, it is defined by the presence of "smoker's macrophages". When manifesting significant clinical symptoms it is referred to as respiratory bronchiolitis interstitial lung disease (RB-ILD).
Tumor-like disorders of the lung pleura are a group of conditions that on initial radiological studies might be confused with malignant lesions. Radiologists must be aware of these conditions in order to avoid misdiagnosing patients. Examples of such lesions are: pleural plaques, thoracic splenosis, catamenial pneumothorax, pleural pseudotumor, diffuse pleural thickening, diffuse pulmonary lymphangiomatosis and Erdheim–Chester disease.
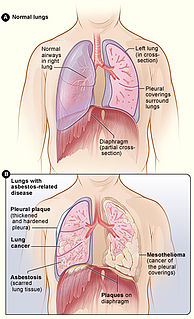
Asbestos-related diseases are disorders of the lung and pleura caused by the inhalation of asbestos fibres. Asbestos-related diseases include non-malignant disorders such as asbestosis, diffuse pleural thickening, pleural plaques, pleural effusion, rounded atelectasis and malignancies such as lung cancer and malignant mesothelioma.
References
- ↑ "Rheumatoid lung disease". Medline Plus Medical Encyclopedia.
- ↑ Chang-Miller, April. "Rheumatoid arthritis: Can it affect the lungs?". MayoClinic. Retrieved 20 February 2017.
- ↑ Nannini, Carlotta; Ryu, Jay; Matteson, Eric. "Lung Disease in Rheumatoid Arthritis". Medscape. Retrieved 20 February 2017.
- ↑ "Rheumatoid lung disease: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2017-12-13.
- ↑ Lang, Florian (2009-03-19). Encyclopedia of Molecular Mechanisms of Disease. Springer Science & Business Media. ISBN 9783540671367.
- 1 2 3 4 Rangel-Moreno, Javier; Randall, Troy D. (2009). "Rheumatoid Lung Disease". Encyclopedia of Molecular Mechanisms of Disease. Springer, Berlin, Heidelberg. pp. 1857–1858. doi:10.1007/978-3-540-29676-8_3216. ISBN 978-3-540-67136-7.
- ↑ Stanislavsky, Alexandra. "Rheumatoid arthritis (pulmonary manifestations) | Radiology Reference Article | Radiopaedia.org". radiopaedia.org. Retrieved 2017-12-13.
- ↑ "Interstitial lung disease - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2017-12-13.
- ↑ Bongartz, Tim; Nannini, Carlotta; Medina-Velasquez, Yimy F.; Achenbach, Sara J.; Crowson, Cynthia S.; Ryu, Jay H.; Vassallo, Robert; Gabriel, Sherine E.; Matteson, Eric L. (June 2010). "Incidence and Mortality of Interstitial Lung Disease in Rheumatoid Arthritis: A Population Based Study". Arthritis and Rheumatism. 62 (6): 1583–1591. doi:10.1002/art.27405. ISSN 0004-3591. PMC 4028137 . PMID 20155830.
- ↑ MIALL WE, CAPLAN A, COCHRANE AL, KILPATRICK GS, OLDHAM PD. An epidemiological study of rheumatoid arthritis associated with characteristic chest x-ray appearances in coal-workers. Br Med J. 1953;2(4848):1231-1236. doi:10.1136/bmj.2.4848.1231
- ↑ "Round 16: Rheumatoid Lung Disease • Arthritis Information". Arthritis Information (in American English). Retrieved 2017-12-13.
- ↑ "Study Explores Risk Factors for RA-Associated Interstitial Lung Disease". MD Magazine. Retrieved 2017-12-13.