Electroconvulsive therapy (ECT) or electroshock therapy (EST) is a psychiatric treatment where a generalized seizure is electrically induced to manage refractory mental disorders. Typically, 70 to 120 volts are applied externally to the patient's head, resulting in approximately 800 milliamperes of direct current passing between the electrodes, for a duration of 100 milliseconds to 6 seconds, either from temple to temple or from front to back of one side of the head. However, only about 1% of the electrical current crosses the bony skull into the brain because skull impedance is about 100 times higher than skin impedance.
Aversion therapy is a form of psychological treatment in which the patient is exposed to a stimulus while simultaneously being subjected to some form of discomfort. This conditioning is intended to cause the patient to associate the stimulus with unpleasant sensations with the intention of quelling the targeted behavior.

Ugo Cerletti was an Italian neurologist who discovered the method of electroconvulsive therapy (ECT) used in psychiatry. Electroconvulsive therapy is a therapy in which electric current is used to provoke a seizure for a short duration. This therapy is used in an attempt to treat certain mental disorders, and may be useful when other possible treatments have not, or cannot, cure the person of their mental disorder.

Manfred Joshua Sakel was an Austrian-Jewish neurophysiologist and psychiatrist, credited with developing insulin shock therapy in 1927.

Ladislas Joseph Meduna was a Hungarian neuropathologist and neuropsychiatrist who initiated convulsive treatment, the repeated induction of grand mal seizures, as a treatment of psychosis. Observing the high concentration of glia in post-mortem brains of patients with epilepsy and a paucity in those with schizophrenia, he proposed that schizophrenia might be treated by inducing "epileptic" seizures. Thus, chemically induced seizures became the electroconvulsive therapy that is now in worldwide use.
Oneirophrenia is a hallucinatory, dream-like state caused by several conditions such as prolonged sleep deprivation, sensory deprivation, or drugs. Oneirophrenia is often confused with an acute case of schizophrenia due to the onset of hallucinations. The severity of this condition can range from derealization to complete hallucinations and delusions. Oneirophrenia was described for the first time in the 1950s but was studied more in the 1960s. Although it is still cited in diagnostic manuals of psychiatry, such as DSM-IV and in the International Statistical Classification of Diseases and Related Health Problems (ICD), oneirophrenia as a separate entity is out of fashion nowadays.
William Walters Sargant was a British psychiatrist who is remembered for the evangelical zeal with which he promoted treatments such as psychosurgery, deep sleep treatment, electroconvulsive therapy and insulin shock therapy.
Psychic driving was a psychiatric procedure of the 1950s and 1960s in which patients were subjected to a continuously repeated audio message on a looped tape to alter their behaviour. In psychic driving, patients were often exposed to hundreds of thousands of repetitions of a single statement over the course of their treatment. They were also concurrently administered muscular paralytic drugs such as curare to subdue them for the purposes of exposure to the looped message(s). The procedure was pioneered by Donald Ewen Cameron, and used and funded by the CIA's Project MKUltra program in Canada.

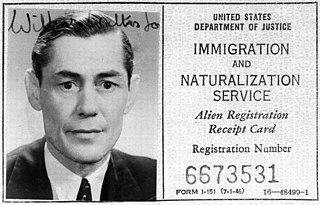
Insulin shock therapy or insulin coma therapy was a form of psychiatric treatment in which patients were repeatedly injected with large doses of insulin in order to produce daily comas over several weeks. It was introduced in 1927 by Austrian-American psychiatrist Manfred Sakel and used extensively in the 1940s and 1950s, mainly for schizophrenia, before falling out of favour and being replaced by neuroleptic drugs in the 1960s.
Deep sleep therapy (DST), also called prolonged sleep treatment or continuous narcosis, is a discredited form of ostensibly psychiatric treatment in which drugs are used to keep patients unconscious for a period of days or weeks. The controversial practice led to the death of 25 patients in Chelmsford Private Hospital in New South Wales, Australia, from the early 1960s to late 1970s.

Lauretta Bender was an American child neuropsychiatrist known for developing the Bender-Gestalt Test, a psychological test designed to evaluate visual-motor maturation in children. First published by Bender in 1938, the test became widely used for assessing children's neurological function and screening for developmental disorders.

The Judge Rotenberg Center (JRC) is a controversial institution in Canton, Massachusetts, United States, for people with developmental disabilities and emotional and behavioral disorders. The center has been condemned for torture by the United Nations special rapporteur on torture. The JRC is known for its use of the graduated electronic decelerator (GED), a device that administers electric shocks to residents as part of the institution's behavior modification program.
Electroconvulsive therapy is a controversial psychiatric treatment in which seizures are induced with electricity. ECT was first used in the United Kingdom in 1939 and, although its use has been declining for several decades, it was still given to about 11,000 people a year in the early 2000s.
Abram Elting Bennett (1898–1985) was an American psychiatrist best known for his work on electroconvulsive therapy (ECT).

Esther Somerfeld-Ziskind was an American neurologist and psychiatrist. She conducted pioneering research into the use of insulin, lithium, and electroconvulsive therapy in the treatment of psychiatric disorders. She was the daughter of Czech and Romanian immigrants. She received her medical degree in Chicago, Illinois, and her Masters in Los Angeles, California. After marrying Eugene Ziskind, they opened their own practice. Somerfeld-Ziskind was later chair of the psychiatry department at Cedars-Sinai Medical Center.

Pentylenetetrazol, also known as pentylenetetrazole, leptazol, metrazol, pentetrazol (INN), pentamethylenetetrazol, Corazol, Cardiazol, Deumacard, or PTZ, is a drug formerly used as a circulatory and respiratory stimulant. High doses cause convulsions, as discovered by Hungarian-American neurologist and psychiatrist Ladislas J. Meduna in 1934. It has been used in convulsive therapy, and was found to be effective—primarily for depression—but side effects such as uncontrolled seizures were difficult to avoid. In 1939, pentylenetetrazol was replaced by electroconvulsive therapy, which is easier to administer, as the preferred method for inducing seizures in England's mental hospitals. In the US, its approval by the Food and Drug Administration was revoked in 1982. It is used in Italy as a cardio-respiratory stimulant in combination with codeine in a cough suppressant drug.

David John Impastato was an American neuropsychiatrist who pioneered the use of electroconvulsive therapy (ECT) in the United States. A treatment for mental illness initially called "electroshock," ECT was developed in 1937 by Dr. Ugo Cerletti and Lucio Bini, working in Rome. Impastato has been credited with the earliest documented use of the revolutionary method in North America, administered in early 1940 to a schizophrenic female patient in New York City. Soon after, he and colleague Dr. Renato Almansi completed the first case study of ECT to appear in a U.S. publication. Impastato spent the next four decades refining the technique, gaining recognition as one of its most authoritative spokesmen. He taught, lectured widely and published over fifty articles on his work. He called on ECT practitioners to observe the strictest protocols of patient safety, countered resistance to ECT from both the medical and cultural establishments, and met later challenges to electroconvulsive therapy from developments in psychopharmacology. Impastato would live to see ECT recommended by the American Psychiatric Association for a distinct core of intractable mental disorders. The U.S. Food and Drug Administration took longer to respond to the treatment's potential. But in 2016 the FDA drafted guidelines for ECT similar to those of the APA, as well as proposing regulations for treatment with Class II and Class III devices. Though still not free of controversy, electroconvulsive therapy is the treatment of choice for an estimated 100,000 patients a year in the United States.
Electroconvulsive therapy (ECT) is a controversial therapy used to treat certain mental illnesses such as major depressive disorder, schizophrenia, depressed bipolar disorder, manic excitement, and catatonia. These disorders are difficult to live with and often very difficult to treat, leaving individuals suffering for long periods of time. In general, ECT is not looked at as a first line approach to treating a mental disorder, but rather a last resort treatment when medications such as antidepressants are not helpful in reducing the clinical manifestations.
The Montreal experiments were a series of experiments, initially aimed to treat schizophrenia by changing memories and erasing the patients' thoughts using the Scottish psychiatrist Donald Ewen Cameron's method of "psychic driving", as well as drug-induced sleep, intensive electroconvulsive therapy, sensory deprivation and Thorazine. The experiments were conducted at the Allan Memorial Institute of McGill University between 1957 and 1964 by Cameron and funded by the CIA as part of Project MKUltra, which lasted until 1973 and was only revealed to the public in 1975.

The graduated electronic decelerator (GED) is a torture device that delivers powerful electric shocks to the skin, described by the United Nations as torture, created by Matthew Israel for use on people at the Judge Rotenberg Center as part of the institution's behavior modification program. The school has since been condemned for torture by the United Nations special rapporteur on torture for its use of the GED and other inhumane punishments. In 2020, the device was banned in the United States by the Food and Drug Administration, however the ban was overturned in federal court a year later. In response, the United States Congress amended the Food, Drug, and Cosmetic Act to expand FDA's authority to ban such devices.