Otorhinolaryngology is a surgical subspecialty within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians. Patients seek treatment from an otorhinolaryngologist for diseases of the ear, nose, throat, base of the skull, head, and neck. These commonly include functional diseases that affect the senses and activities of eating, drinking, speaking, breathing, swallowing, and hearing. In addition, ENT surgery encompasses the surgical management of cancers and benign tumors and reconstruction of the head and neck as well as plastic surgery of the face, scalp, and neck.

Sleep apnea is a sleep-related breathing disorder in which repetitive pauses in breathing, periods of shallow breathing, or collapse of the upper airway during sleep results in poor ventilation and sleep disruption. Each pause in breathing can last for a few seconds to a few minutes and occurs many times a night. A choking or snorting sound may occur as breathing resumes. Common symptoms include daytime sleepiness, snoring, and non restorative sleep despite adequate sleep time. Because the disorder disrupts normal sleep, those affected may experience sleepiness or feel tired during the day. It is often a chronic condition.

Snoring is the vibration of respiratory structures and the resulting sound due to obstructed air movement during breathing while sleeping. The sound may be soft or loud and unpleasant. Snoring during sleep may be a sign, or first alarm, of obstructive sleep apnea (OSA). Research suggests that snoring is one of the factors of sleep deprivation.

Obesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.
Upper airway resistance syndrome (UARS) is a sleep disorder characterized by the narrowing of the airway that can cause disruptions to sleep. The symptoms include unrefreshing sleep, fatigue, sleepiness, chronic insomnia, and difficulty concentrating. UARS can be diagnosed by polysomnograms capable of detecting Respiratory Effort-related Arousals. It can be treated with lifestyle changes, functional orthodontics, surgery, mandibular repositioning devices or CPAP therapy. UARS is considered a variant of sleep apnea, although some scientists and doctors believe it to be a distinct disorder.
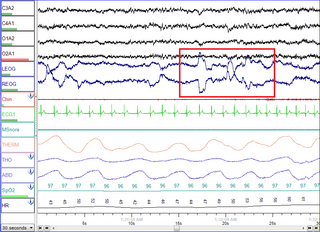
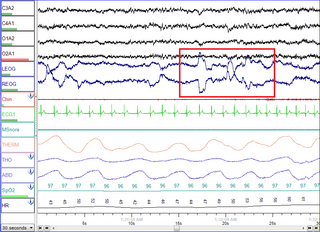
Polysomnography (PSG) is a multi-parameter type of sleep study and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.

A mandibi splint or mandibi advancement splint is a prescription custom-made medical device worn in the mouth used to treat sleep-related breathing disorders including: obstructive sleep apnea (OSA), snoring, and TMJ disorders. These devices are also known as mandibular advancement devices, sleep apnea oral appliances, oral airway dilators, and sleep apnea mouth guards.

Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episodes are termed "apneas" with complete or near-complete cessation of breathing, or "hypopneas" when the reduction in breathing is partial. In either case, a fall in blood oxygen saturation, a disruption in sleep, or both, may result. A high frequency of apneas or hypopneas during sleep may interfere with the quality of sleep, which – in combination with disturbances in blood oxygenation – is thought to contribute to negative consequences to health and quality of life. The terms obstructive sleep apnea syndrome (OSAS) or obstructive sleep apnea–hypopnea syndrome (OSAHS) may be used to refer to OSA when it is associated with symptoms during the daytime.

Somnology is the scientific study of sleep. It includes clinical study and treatment of sleep disorders and irregularities. Sleep medicine is a subset of somnology.

Uvulopalatopharyngoplasty is a surgical procedure or sleep surgery used to remove tissue and/or remodel tissue in the throat. This could be because of sleep issues. Tissues which may typically be removed include:
Mouth breathing, medically known as chronic oral ventilation, is long-term breathing through the mouth. It often is caused by an obstruction to breathing through the nose, the innate breathing organ in the human body. However, by the early 20th century, the term "mouth-breather" had developed a pejorative slang meaning connoting a stupid person.
Hypopnea is overly shallow breathing or an abnormally low respiratory rate. Hypopnea is defined by some to be less severe than apnea, while other researchers have discovered hypopnea to have a "similar if not indistinguishable impact" on the negative outcomes of sleep breathing disorders. In sleep clinics, obstructive sleep apnea syndrome or obstructive sleep apnea–hypopnea syndrome is normally diagnosed based on the frequent presence of apneas and/or hypopneas rather than differentiating between the two phenomena. Hypopnea is typically defined by a decreased amount of air movement into the lungs and can cause oxygen levels in the blood to drop. It commonly is due to partial obstruction of the upper airway.
Pharyngeal flap surgery is a procedure to correct the airflow during speech. The procedure is common among people with cleft palate and some types of dysarthria.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.
Uvulopalatoplasty is a surgical procedure performed with the aim of reducing or eliminating snoring. It is an out-patient procedure, in which a laser is used to remove parts or all of the uvula at the rear of the mouth. The surgery usually requires three to five visits, with each lasting less than 30 minutes. It is performed with the patient awake under local anesthesia, and normal functions can be resumed after the operation. An LAUP procedure typically costs between two and three thousand American dollars. The principal side effect is a severe sore throat which can last from 7 – 10 days. Speaking is not usually affected. Typically a CO2 type laser is used.

Heated humidified high-flow therapy, often simply called high flow therapy, is a type of respiratory support that delivers a flow of medical gas to a patient of up to 60 liters per minute and 100% oxygen through a large bore or high flow nasal cannula. Primarily studied in neonates, it has also been found effective in some adults to treat hypoxemia and work of breathing issues. The key components of it are a gas blender, heated humidifier, heated circuit, and cannula.
Nasal expiratory positive airway pressure is a treatment for obstructive sleep apnea (OSA) and snoring.
Sleep surgery is a surgery performed to treat sleep disordered breathing. Sleep disordered breathing is a spectrum of disorders that includes snoring, upper airway resistance syndrome, and obstructive sleep apnea. These surgeries are performed by surgeons trained in otolaryngology, oral maxillofacial surgery, and craniofacial surgery.
Hyoid suspension, also known as hyoid myotomy and suspension or hyoid advancement, is a surgical procedure or sleep surgery in which the hyoid bone and its muscle attachments to the tongue and airway are pulled forward with the aim of increasing airway size and improving airway stability in the retrolingual and hypopharyngeal airway. The horseshoe shaped hyoid bone sits directly below the base of tongue with the arms of the bone flanking the airway. Hyoid suspension is typically performed as a treatment for obstructive sleep apnea (OSA). This procedure is frequently performed with a uvulopalatopharyngoplasty (UPPP) which targets sites of obstruction higher in the airway. Typically, a hyoid suspension is considered successful when the patient's apnea-hypopnea index is significantly reduced after surgery.