In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

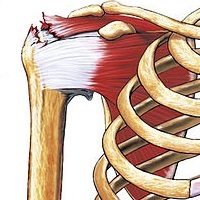
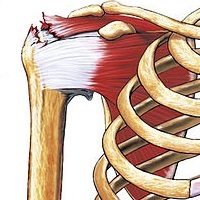
Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

Back injuries result from damage, wear, or trauma to the bones, muscles, or other tissues of the back. Common back injuries include sprains and strains, herniated discs, and fractured vertebrae. The lumbar spine is often the site of back pain. The area is susceptible because of its flexibility and the amount of body weight it regularly bears. It is estimated that low-back pain may affect as much as 80 to 90 percent of the general population in the United States.

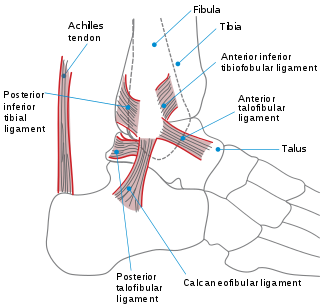
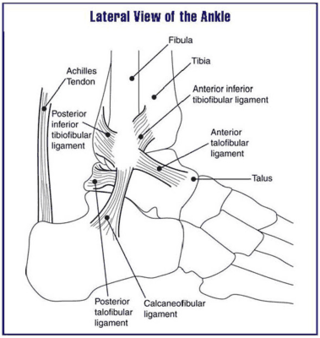
Achilles tendinitis, also known as achilles tendinopathy, occurs when the Achilles tendon, found at the back of the ankle, becomes sore. Achilles tendinopathy is accompanied by alterations in the tendon's structure and mechanical properties. The most common symptoms are pain and swelling around the affected tendon. The pain is typically worse at the start of exercise and decreases thereafter. Stiffness of the ankle may also be present. Onset is generally gradual.
A soft tissue injury is the damage of muscles, ligaments and tendons throughout the body. Common soft tissue injuries usually occur from a sprain, strain, a one-off blow resulting in a contusion or overuse of a particular part of the body. Soft tissue injuries can result in pain, swelling, bruising and loss of function.

Achilles tendon rupture is when the Achilles tendon, at the back of the ankle, breaks. Symptoms include the sudden onset of sharp pain in the heel. A snapping sound may be heard as the tendon breaks and walking becomes difficult.

Tarsal tunnel syndrome (TTS) is a nerve entrapment syndrome causing a painful foot condition in which the tibial nerve is compressed as it travels through the tarsal tunnel. This tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.

A strain is an acute or chronic soft tissue injury that occurs to a muscle, tendon, or both. The equivalent injury to a ligament is a sprain. Generally, the muscle or tendon overstretches and partially tears, under more physical stress than it can withstand, often from a sudden increase in duration, intensity, or frequency of an activity. Strains most commonly occur in the foot, leg, or back. Immediate treatment typically includes five steps abbreviated as P.R.I.C.E.: protection, rest, ice, compression, elevation.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.
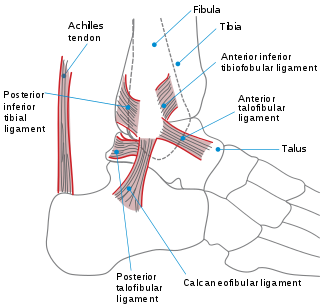
A sprained ankle is an injury where sprain occurs on one or more ligaments of the ankle. It is the most commonly occurring injury in sports, mainly in ball sports such as basketball, volleyball, football, and tennis.

An anterior cruciate ligament injury occurs when the anterior cruciate ligament (ACL) is either stretched, partially torn, or completely torn. The most common injury is a complete tear. Symptoms include pain, an audible cracking sound during injury, instability of the knee, and joint swelling. Swelling generally appears within a couple of hours. In approximately 50% of cases, other structures of the knee such as surrounding ligaments, cartilage, or meniscus are damaged.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.

Jammed finger is a colloquialism referring to a variety of injuries to the joints of the fingers, resulting from axial loading beyond that which the ligaments can withstand. Common parts of the finger susceptible to this type of injury are ligaments, joints, and bones. The severity of the damage to the finger increases with the magnitude of the force exerted by the external object on the fingertip. Toes may become jammed as well, with similar results.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
A high ankle sprain, also known as a syndesmotic ankle sprain (SAS), is a sprain of the syndesmotic ligaments that connect the tibia and fibula in the lower leg, thereby creating a mortise and tenon joint for the ankle. High ankle sprains are described as high because they are located above the ankle. They comprise approximately 15% of all ankle sprains. Unlike the common lateral ankle sprains, when ligaments around the ankle are injured through an inward twisting, high ankle sprains are caused when the lower leg and foot externally rotates.
Musculoskeletal injury refers to damage of muscular or skeletal systems, which is usually due to a strenuous activity and includes damage to skeletal muscles, bones, tendons, joints, ligaments, and other affected soft tissues. In one study, roughly 25% of approximately 6300 adults received a musculoskeletal injury of some sort within 12 months—of which 83% were activity-related. Musculoskeletal injury spans into a large variety of medical specialties including orthopedic surgery, sports medicine, emergency medicine and rheumatology.

Knee pain is pain in or around the knee.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:
Running injuries affect about half of runners annually. The frequencies of various RRI depend on the type of running, such as speed and mileage. Some injuries are acute, caused by sudden overstress, such as side stitch, strains, and sprains. Many of the common injuries that affect runners are chronic, developing over longer periods as the result of overuse. Common overuse injuries include shin splints, stress fractures, Achilles tendinitis, Iliotibial band syndrome, Patellofemoral pain, and plantar fasciitis.
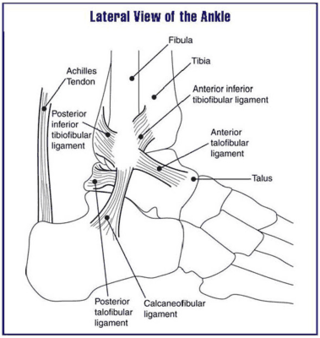
Ankle problems occur frequently, having symptoms of pain or discomfort in the ankles.