Related Research Articles

A pharmacist, also known as a chemist or a druggist, is a healthcare professional who dispenses medications and who provides advice on their effective use, with the aim of preventing disease and promoting public health. Pharmacists often serve as primary care providers in the community, and may offer other services such as health screenings and immunizations.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered health-care professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin: Recipere, that gave the list of the materials to be compounded.
Prescription drug list prices in the United States continually rank among the highest in the world. The high cost of prescription drugs became a major topic of discussion in the 21st century, leading up to the American health care reform debate of 2009, and received renewed attention in 2015. One major reason for high prescription drug prices in the United States relative to other countries is the inability of government-granted monopolies in the American health care sector to use their bargaining power to negotiate lower prices and that the American payer ends up subsidizing the world's R&D spending on drugs.
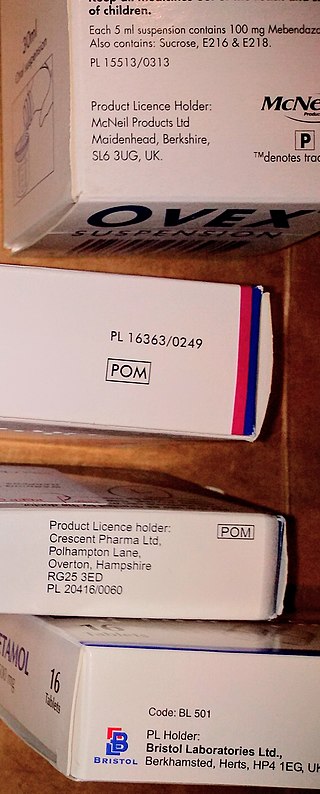
A prescription drug is a pharmaceutical drug that is only permitted to be dispensed to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.

Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs. Part D was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. Under the program, drug benefits are provided by private insurance plans that receive premiums from both enrollees and the government. Part D plans typically pay most of the cost for prescriptions filled by their enrollees. However, plans are later reimbursed for much of this cost through rebates paid by manufacturers and pharmacies.
In medicine, patient compliance describes the degree to which a patient correctly follows medical advice. Most commonly, it refers to medication or drug compliance, but it can also apply to other situations such as medical device use, self care, self-directed exercises, or therapy sessions. Both patient and health-care provider affect compliance, and a positive physician-patient relationship is the most important factor in improving compliance. Access to care plays a role in patient adherence, whereby greater wait times to access care contributing to greater absenteeism. The cost of prescription medication also plays a major role.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.

Clinical pharmacy is the branch of pharmacy in which clinical pharmacists provide direct patient care that optimizes the use of medication and promotes health, wellness, and disease prevention. Clinical pharmacists care for patients in all health care settings but the clinical pharmacy movement initially began inside hospitals and clinics. Clinical pharmacists often work in collaboration with physicians, physician assistants, nurse practitioners, and other healthcare professionals. Clinical pharmacists can enter into a formal collaborative practice agreement with another healthcare provider, generally one or more physicians, that allows pharmacists to prescribe medications and order laboratory tests.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
Medication costs, also known as drug costs are a common health care cost for many people and health care systems. Prescription costs are the costs to the end consumer. Medication costs are influenced by multiple factors such as patents, stakeholder influence, and marketing expenses. A number of countries including Canada, parts of Europe, and Brazil use external reference pricing as a means to compare drug prices and to determine a base price for a particular medication. Other countries use pharmacoeconomics, which looks at the cost/benefit of a product in terms of quality of life, alternative treatments, and cost reduction or avoidance in other parts of the health care system. Structures like the UK's National Institute for Health and Clinical Excellence and to a lesser extent Canada's Common Drug Review evaluate products in this way.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
There are approximately 88,000 pharmacies in the United States. Over half are located within drug stores, grocery stores, hospitals, department stores, medical clinics, surgery clinics, universities, nursing homes, prisons, and other facilities. The remaining pharmacies are considered to be independent or privately owned. The top 25 pharmacy chain stores represent about 38,000 pharmacy locations in the U.S. and employ about 149,000 on-staff pharmacists. California has 8,015 pharmacies, the most of any state. Texas, Florida, New York, and Pennsylvania round out the top five states for pharmacy locations. Nationwide, the number of community pharmacies increased by 6.3% between 2007-2015, and the number of pharmacies per 10,000 people (2.11) did not change. However, the number of pharmacies per-capita varies substantially across counties, ranging from 0 to 13.6 per- 10,000 people in 2015.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.
Prior authorization is a utilization management process used by some health insurance companies in the United States to determine if they will cover a prescribed procedure, service, or medication. The process is intended to act as a safety and cost-saving measure although it has received criticism from physicians for being costly and time-consuming.
Specialty drugs or specialty pharmaceuticals are a recent designation of pharmaceuticals that are classified as high-cost, high complexity and/or high touch. Specialty drugs are often biologics—"drugs derived from living cells" that are injectable or infused. They are used to treat complex or rare chronic conditions such as cancer, rheumatoid arthritis, hemophilia, H.I.V. psoriasis, inflammatory bowel disease and hepatitis C. In 1990 there were 10 specialty drugs on the market, in the mid-1990s there were fewer than 30, by 2008 there were 200, and by 2015 there were 300. Drugs are often defined as specialty because their price is much higher than that of non-specialty drugs. Medicare defines any drug for which the negotiated price is $670 per month or more, as a specialty drug which is placed in a specialty tier that requires a higher patient cost sharing. Drugs are also identified as specialty when there is a special handling requirement or the drug is only available via a limited distributions network. By 2015 "specialty medications accounted for one-third of all spending on drugs in the United States, up from 19 percent in 2004 and heading toward 50 percent in the next 10 years", according to IMS Health, which tracks prescriptions. According to a 2010 article in Forbes, specialty drugs for rare diseases became more expensive "than anyone imagined" and their success came "at a time when the traditional drug business of selling medicines to the masses" was "in decline". In 2015 analysis by The Wall Street Journal suggested the large premium was due to the perceived value of rare disease treatments which usually are very expensive when compared to treatments for more common diseases.
Specialty pharmacy refers to distribution channels designed to handle specialty drugs — pharmaceutical therapies that are either high cost, high complexity and/or high touch. High touch refers to higher degree of complexity in terms of distribution, administration, or patient management which drives up the cost of the drugs. In the early years specialty pharmacy providers attached "high-touch services to their overall price tags" arguing that patients who receive specialty pharmaceuticals "need high levels of ancillary and follow-up care to ensure that the drug spend is not wasted on them." An example of a specialty drug that would only be available through specialty pharmacy is interferon beta-1a (Avonex), a treatment for MS that requires a refrigerated chain of distribution and costs $17,000 a year. Some specialty pharmacies deal in pharmaceuticals that treat complex or rare chronic conditions such as cancer, rheumatoid arthritis, hemophilia, H.I.V. psoriasis, inflammatory bowel disease (IBD) or Hepatitis C. "Specialty pharmacies are seen as a reliable distribution channel for expensive drugs, offering patients convenience and lower costs while maximizing insurance reimbursements from those companies that cover the drug. Patients typically pay the same co-payments whether or not their insurers cover the drug." As the market demanded specialization in drug distribution and clinical management of complex therapies, specialized pharma (SP) evolved.„ Specialty pharmacies may handle therapies that are biologics, and are injectable or infused. By 2008 the pharmacy benefit management dominated the specialty pharmacies market having acquired smaller specialty pharmacies. PBMs administer specialty pharmacies in their network and can "negotiate better prices and frequently offer a complete menu of specialty pharmaceuticals and related services to serve as an attractive 'one-stop shop' for health plans and employers."
A collaborative practice agreement (CPA) is a legal document in the United States that establishes a legal relationship between clinical pharmacists and collaborating physicians that allows for pharmacists to participate in collaborative drug therapy management (CDTM).

Drug utilization review refers to a review of prescribing, dispensing, administering and ingesting of medication. This authorized, structured and ongoing review is related to pharmacy benefit managers. Drug use/ utilization evaluation and medication utilization evaluations are the same as drug utilization review.
References
- ↑ Jessica S. Banthin, Peter Cunningham, and Didem M. Bernard "Financial Burden Of Health Care", 2001–2004 Health Affairs, January/February 2008; 27(1): 188-195.
- ↑ Brenda R. Motheral, PhD; Rochelle Henderson, MPA; and Emily R. Cox, PhD "Investigation showing step therapy reduces managed care costs: Plan-Sponsor Savings and Member Experience With Point-of-Service Prescription Step Therapy", The American Journal of Managed Care Volume 10:457-464 July 2004 Number 7 Pt 1
- ↑ Neil J. MacKinnon, Ph.D., R.Ph., Ritu Kumar, M.H.S.A., R.N., "Prior Authorization Programs: A Critical Review of the Literature", Journal of Managed Care Pharmacy 2001 Volume 7 Issue 4:297-303
- ↑ FailFirstHurts.org