Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.
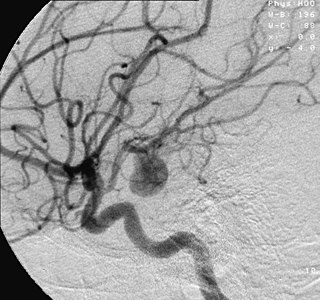
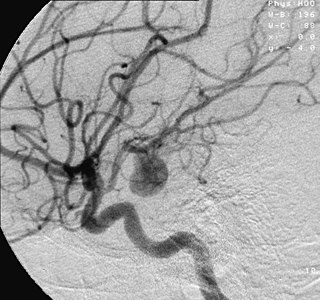
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus for clot formation (thrombosis) and embolization. As an aneurysm increases in size, the risk of rupture, which leads to uncontrolled bleeding, increases. Although they may occur in any blood vessel, particularly lethal examples include aneurysms of the circle of Willis in the brain, aortic aneurysms affecting the thoracic aorta, and abdominal aortic aneurysms. Aneurysms can arise in the heart itself following a heart attack, including both ventricular and atrial septal aneurysms. There are congenital atrial septal aneurysms, a rare heart defect.

An anastomosis is a connection or opening between two things that are normally diverging or branching, such as between blood vessels, leaf veins, or streams. Such a connection may be normal or abnormal ; it may be acquired or innate ; and it may be natural or artificial. The reestablishment of an anastomosis that had become blocked is called a reanastomosis. Anastomoses that are abnormal, whether congenital or acquired, are often called fistulas.

A stapler is a mechanical device that joins pages of paper or similar material by driving a thin metal staple through the sheets and folding the ends. Staplers are widely used in government, business, offices, work places, homes and schools.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

Microsurgery is a general term for surgery requiring an operating microscope. The most obvious developments have been procedures developed to allow anastomosis of successively smaller blood vessels and nerves which have allowed transfer of tissue from one part of the body to another and re-attachment of severed parts. Microsurgical techniques are utilized by several specialties today, such as general surgery, ophthalmology, orthopedic surgery, gynecological surgery, otolaryngology, neurosurgery, oral and maxillofacial surgery, endodontic microsurgery, plastic surgery, podiatric surgery and pediatric surgery.

A surgical instrument is a medical device for performing specific actions or carrying out desired effects during a surgery or operation, such as modifying biological tissue, or to provide access for viewing it. Over time, many different kinds of surgical instruments and tools have been invented. Some surgical instruments are designed for general use in all sorts of surgeries, while others are designed for only certain specialties or specific procedures.
A vascular bypass is a surgical procedure performed to redirect blood flow from one area to another by reconnecting blood vessels. Often, this is done to bypass around a diseased artery, from an area of normal blood flow to another relatively normal area. It is commonly performed due to inadequate blood flow (ischemia) caused by atherosclerosis, as a part of organ transplantation, or for vascular access in hemodialysis. In general, someone's own vein (autograft) is the preferred graft material for a vascular bypass, but other types of grafts such as polytetrafluoroethylene (Teflon), polyethylene terephthalate (Dacron), or a different person's vein (allograft) are also commonly used. Arteries can also serve as vascular grafts. A surgeon sews the graft to the source and target vessels by hand using surgical suture, creating a surgical anastomosis.

A surgical anastomosis is a surgical technique used to make a new connection between two body structures that carry fluid, such as blood vessels or bowel. For example, an arterial anastomosis is used in vascular bypass and a colonic anastomosis is used to restore colonic continuity after the resection of colon cancer.

Endovascular aneurysm repair (EVAR) is a type of minimally-invasive endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA). When used to treat thoracic aortic disease, the procedure is then specifically termed TEVAR for "thoracic endovascular aortic/aneurysm repair." EVAR involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta. In 2003, EVAR surpassed open aortic surgery as the most common technique for repair of AAA, and in 2010, EVAR accounted for 78% of all intact AAA repair in the United States.
Cardiothoracic anesthesiology is a subspeciality of the medical practice of anesthesiology, devoted to the preoperative, intraoperative, and postoperative care of adult and pediatric patients undergoing cardiothoracic surgery and related invasive procedures.

John Benjamin Murphy, born John Murphy was an American physician and abdominal surgeon noted for advocating early surgical intervention in appendicitis appendectomy, and several eponyms: Murphy’s button, Murphy drip, Murphy’s punch, Murphy’s test, and Murphy-Lane bone skid. He is best remembered for the eponymous clinical sign that is used in evaluating patients with acute cholecystitis. His career spanned general surgery, orthopedics, neurosurgery, and cardiothoracic surgery, which helped him to gain international prominence in the surgical profession. Mayo Clinic co-founder William James Mayo called him "the surgical genius of our generation".

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

Félicien M. Steichen was a Luxembourgish-born American surgeon and Professor of Surgery. He was a pioneer in the development and use of surgical staples. He and Mark M. Ravitch are considered the fathers of modern surgical stapling. Steichen was also noted for his contributions to the development of minimally-invasive surgery.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.
Vasilii Ivanovich Kolesov was one of the pioneers of global cardiac surgery. He was the first to perform successful internal coronary artery bypass surgery using mammary artery–coronary artery anastomosis in 1964. Also in 1964, he performed the first successful coronary bypass using a standard suture technique. Kolesov was a recipient of the USSR State Prize and Honoured Worker of Science of the RSFSR (1964).

Hümér Hültl was a Hungarian surgeon, noted for his work with surgical staples.

Dr. Anil Bhan is the Chairman of Cardiac Surgery Heart Institute, Medanta Hospital, Gurugram, India. He graduated from Medical College Srinagar. He has the largest experience in aortic surgery in India since he has designed and developed more than 50 surgical instruments in the field of cardiac surgery. He was one of the team members to perform the first successful heart transplant in India in1994. He served as a co-founder of Max Heart and Vascular Institute, Saket, New Delhi, Director and Chief Co-Ordinator, Cardio thoracic and Vascular Surgery, MHVI, Saket.Additional Professor, Cardiothoracic Surgery and Vascular Surgery, AIIMS, New Delhi.

George E. Green is an American cardiac surgeon best known for pioneering and implementing the first surgical procedure of the left coronary artery bypass graft using the internal thoracic artery sutured to the left anterior descending coronary artery to bypass obstruction to the heart circulation in the late 1960s. He applied these techniques in 1968 at New York University Medical Center. In 1970 he was hired to establish St. Luke's Hospital's cardiac surgery program in Manhattan, New York, which by 1982 was seeing approximately 1,800 cases a year, the biggest program in the state. Green has lectured internationally on the topic, and has written numerous reports on internal thoracic artery grafting, as well as co-authoring Surgical Revascularization of the Heart: The Internal Thoracic Arteries.

Antrectomy, also called distal gastrectomy, is a type of gastric resection surgery that involves the removal of the stomach antrum to treat gastric diseases causing the damage, bleeding, or blockage of the stomach. This is performed using either the Billroth I (BI) or Billroth II (BII) reconstruction method. Quite often, antrectomy is used alongside vagotomy to maximise its safety and effectiveness. Modern antrectomies typically have a high success rate and low mortality rate, but the exact numbers depend on the specific conditions being treated.