Related Research Articles

Malaria is a mosquito-borne infectious disease that affects humans and other animals. Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. Symptoms usually begin ten to fifteen days after being bitten by an infected mosquito. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to malaria.
Antimalarial medications or simply antimalarials are a type of antiparasitic chemical agent, often naturally derived, that can be used to treat or to prevent malaria, in the latter case, most often aiming at two susceptible target groups, young children and pregnant women. As of 2018, modern treatments, including for severe malaria, continued to depend on therapies deriving historically from quinine and artesunate, both parenteral (injectable) drugs, expanding from there into the many classes of available modern drugs. Incidence and distribution of the disease is expected to remain high, globally, for many years to come; moreover, known antimalarial drugs have repeatedly been observed to elicit resistance in the malaria parasite—including for combination therapies featuring artemisinin, a drug of last resort, where resistance has now been observed in Southeast Asia. As such, the needs for new antimalarial agents and new strategies of treatment remain important priorities in tropical medicine. As well, despite very positive outcomes from many modern treatments, serious side effects can impact some individuals taking standard doses.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

Varicella-zoster virus (VZV), also known as human herpesvirus 3 or Human alphaherpesvirus 3 (taxonomically), is one of nine known herpes viruses that can infect humans. It causes chickenpox (varicella) commonly affecting children and young adults, and shingles in adults but rarely in children. VZV infections are species-specific to humans. The virus can survive in external environments for a few hours.

Shingles, also known as zoster or herpes zoster, is a viral disease characterized by a painful skin rash with blisters in a localized area. Typically the rash occurs in a single, wide mark either on the left or right side of the body or face. Two to four days before the rash occurs there may be tingling or local pain in the area. Otherwise, there are typically few symptoms though some people may have fever or headache, or feel tired. The rash usually heals within two to four weeks; however, some people develop ongoing nerve pain which can last for months or years, a condition called postherpetic neuralgia (PHN). In those with poor immune function the rash may occur widely. If the rash involves the eye, vision loss may occur.

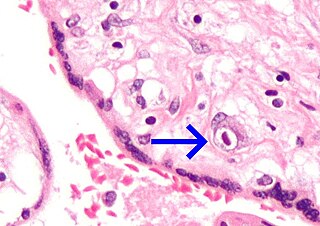
Plasmodium falciparum is a unicellular protozoan parasite of humans, and the deadliest species of Plasmodium that causes malaria in humans. The parasite is transmitted through the bite of a female Anopheles mosquito and causes the disease's most dangerous form, falciparum malaria. It is responsible for around 50% of all malaria cases. P. falciparum is therefore regarded as the deadliest parasite in humans. It is also associated with the development of blood cancer and is classified as a Group 2A (probable) carcinogen.

Complications of pregnancy are health problems that are related to pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. Severe complications of pregnancy, childbirth, and the puerperium are present in 1.6% of mothers in the US, and in 1.5% of mothers in Canada. In the immediate postpartum period (puerperium), 87% to 94% of women report at least one health problem. Long-term health problems are reported by 31% of women.
A vertically transmitted infection is an infection caused by pathogenic bacteria or viruses that use mother-to-child transmission, that is, transmission directly from the mother to an embryo, fetus, or baby during pregnancy or childbirth. It can occur when the mother has a pre-existing disease or becomes infected during pregnancy. Nutritional deficiencies may exacerbate the risks of perinatal infections. Vertical transmission is important for the mathematical modelling of infectious diseases, especially for diseases of animals with large litter sizes, as it causes a wave of new infectious individuals.
Passive immunity is the transfer of active humoral immunity of ready-made antibodies. Passive immunity can occur naturally, when maternal antibodies are transferred to the fetus through the placenta, and it can also be induced artificially, when high levels of antibodies specific to a pathogen or toxin are transferred to non-immune persons through blood products that contain antibodies, such as in immunoglobulin therapy or antiserum therapy. Passive immunization is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of ongoing or immunosuppressive diseases. Passive immunization can be provided when people cannot synthesize antibodies, and when they have been exposed to a disease that they do not have immunity against.

Chickenpox, or chicken pox, also known as varicella, is a highly contagious disease caused by the initial infection with varicella zoster virus (VZV). The disease results in a characteristic skin rash that forms small, itchy blisters, which eventually scab over. It usually starts on the chest, back, and face. It then spreads to the rest of the body. The rash and other symptoms, such as fever, tiredness, and headaches, usually last five to seven days. Complications may occasionally include pneumonia, inflammation of the brain, and bacterial skin infections. The disease is usually more severe in adults than in children.

Herpes simplex is a viral infection caused by the herpes simplex virus. Infections are categorized based on the part of the body infected.
Neonatal herpes is a rare but serious condition, usually caused by vertical transmission of the herpes simplex virus from mother to newborn. Around 1 in every 3,500 babies in the United States contract the infection.
Immune tolerance in pregnancy or maternal immune tolerance is the immune tolerance shown towards the fetus and placenta during pregnancy. This tolerance counters the immune response that would normally result in the rejection of something foreign in the body, as can happen in cases of spontaneous abortion. It is studied within the field of reproductive immunology.
Pregnancy-associated malaria (PAM) or placental malaria is a presentation of the common illness that is particularly life-threatening to both mother and developing fetus. PAM is caused primarily by infection with Plasmodium falciparum, the most dangerous of the four species of malaria-causing parasites that infect humans. During pregnancy, a woman faces a much higher risk of contracting malaria and of associated complications. Prevention and treatment of malaria are essential components of prenatal care in areas where the parasite is endemic – tropical and subtropical geographic areas. Placental malaria has also been demonstrated to occur in animal models, including in rodent and non-human primate models.

Developmental toxicity is any structural or functional alteration, reversible or irreversible, which interferes with homeostasis, normal growth, differentiation, development or behavior. Developmental toxicity is caused by environmental insult, which includes drugs, alcohol, diet, toxic chemicals, and physical factors. More factors causing developmental toxicity are radiation, infections, maternal metabolic imbalances, drugs, and environmental chemicals .In addition, it is the study of adverse effects on the development of the organism that can result from exposure to toxic agents before conception, during fetal development, or even following birth.
Maternal oral health has been shown to affect the well-being of both the expectant mother and her unborn fetus.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Sanaria is a biotechnology company developing vaccines protective against malaria and other infectious diseases as well as related products for use in malaria research. Sanaria's vaccines are based on the use of the sporozoite (SPZ) stage of the malaria parasite, Plasmodium, as an immunogen, and as a platform technology for liver-vectored gene delivery. SPZ are normally introduced into humans by mosquito bite where they migrate to the liver and further develop to liver stages, and eventually back into the blood stream where the parasite infects red blood cells (RBC) and causes malaria. Plasmodium falciparum is the species responsible for more than 95% deaths caused by malaria. The WHO estimates there were 241 million clinical cases and 627,000 deaths in 2020 alone.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Kourtis, Athena P.; Read, Jennifer S.; Jamieson, Denise J. (2014). "Pregnancy and Infection". New England Journal of Medicine. 370 (23): 2211–2218. doi:10.1056/NEJMra1213566. ISSN 0028-4793. PMC 4459512 . PMID 24897084.
- ↑ Jamieson DJ, Theiler RN, Rasmussen SA. Emerging infections and pregnancy. Emerg Infect Dis. 2006 Nov. Available from https://www.cdc.gov/ncidod/EID/vol12no11/06-0152.htm