Related Research Articles

Catatonia is a complex neuropsychiatric behavioral syndrome that is characterized by abnormal movements, immobility, abnormal behaviors, and withdrawal. The onset of catatonia can be acute or subtle and symptoms can wax, wane, or change during episodes. It has historically been related to schizophrenia, but catatonia is most often seen in mood disorders. It is now known that catatonic symptoms are nonspecific and may be observed in other mental, neurological, and medical conditions. Catatonia is now a stand-alone diagnosis, and the term is used to describe a feature of the underlying disorder.
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.
A communication disorder is any disorder that affects an individual's ability to comprehend, detect, or apply language and speech to engage in dialogue effectively with others. This also encompasses deficiencies in verbal and non-verbal communication styles. The delays and disorders can range from simple sound substitution to the inability to understand or use one's native language. This article covers subjects such as diagnosis, the DSM-IV, the DSM-V, and examples like sensory impairments, aphasia, learning disabilities, and speech disorders.
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal functions are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatigue, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.

Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.
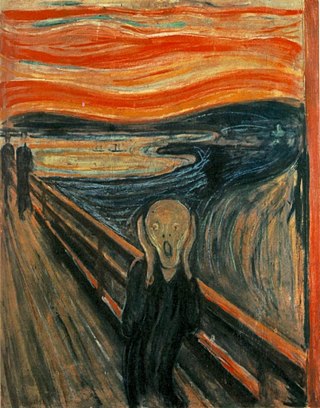
Abnormal psychology is the branch of psychology that studies unusual patterns of behavior, emotion, and thought, which could possibly be understood as a mental disorder. Although many behaviors could be considered as abnormal, this branch of psychology typically deals with behavior in a clinical context. There is a long history of attempts to understand and control behavior deemed to be aberrant or deviant, and there is often cultural variation in the approach taken. The field of abnormal psychology identifies multiple causes for different conditions, employing diverse theories from the general field of psychology and elsewhere, and much still hinges on what exactly is meant by "abnormal". There has traditionally been a divide between psychological and biological explanations, reflecting a philosophical dualism in regard to the mind-body problem. There have also been different approaches in trying to classify mental disorders. Abnormal includes three different categories; they are subnormal, supernormal and paranormal.

A thought disorder (TD) is a disturbance in cognition which affects language, thought and communication. Psychiatric and psychological glossaries in 2015 and 2017 identified thought disorders as encompassing poverty of ideas, neologisms, paralogia, word salad, and delusions—all disturbances of thought content and form. Two specific terms have been suggested—content thought disorder (CTD) and formal thought disorder (FTD). CTD has been defined as a thought disturbance characterized by multiple fragmented delusions, and the term thought disorder is often used to refer to an FTD: a disruption of the form of thought. Also known as disorganized thinking, FTD results in disorganized speech and is recognized as a major feature of schizophrenia and other psychoses. Disorganized speech leads to an inference of disorganized thought. Thought disorders include derailment, pressured speech, poverty of speech, tangentiality, verbigeration, and thought blocking. One of the first known cases of thought disorders, or specifically OCD as it is known today, was in 1691. John Moore, who was a bishop, had a speech in front of Queen Mary II, about "religious melancholy."
In psychology, alogia is poor thinking inferred from speech and language usage. There may be a general lack of additional, unprompted content seen in normal speech, so replies to questions may be brief and concrete, with less spontaneous speech. This is termed poverty of speech or laconic speech. The amount of speech may be normal but conveys little information because it is vague, empty, stereotyped, overconcrete, overabstract, or repetitive. This is termed poverty of content or poverty of content of speech. Under Scale for the Assessment of Negative Symptoms used in clinical research, thought blocking is considered a part of alogia, and so is increased latency in response.

A mood swing is an extreme or sudden change of mood. Such changes can play a positive part in promoting problem solving and in producing flexible forward planning, or be disruptive. When mood swings are severe, they may be categorized as part of a mental illness, such as bipolar disorder, where erratic and disruptive mood swings are a defining feature.
The mental status examination (MSE) is an important part of the clinical assessment process in neurological and psychiatric practice. It is a structured way of observing and describing a patient's psychological functioning at a given point in time, under the domains of appearance, attitude, behavior, mood and affect, speech, thought process, thought content, perception, cognition, insight, and judgment. There are some minor variations in the subdivision of the MSE and the sequence and names of MSE domains.
Disorganized schizophrenia, or hebephrenia, was a subtype of schizophrenia prior to 2013. Subtypes of schizophrenia were no longer recognized as separate conditions in the DSM 5, published in 2013. The disorder is no longer listed in the 11th revision of the International Classification of Diseases (ICD-11).
Acute stress reaction and acute stress disorder (ASD) is a psychological response to a terrifying, traumatic or surprising experience. Combat stress reaction (CSR) is a similar response to the trauma of war. The reactions may include but are not limited to intrusive or dissociative symptoms, and reactivity symptoms such as avoidance or arousal. It may be exhibited for days or weeks after the traumatic event. If the condition is not correctly addressed, it may develop into post-traumatic stress disorder (PTSD).
Thought broadcasting is a type of delusional condition in which the affected person believes that others can hear their inner thoughts, despite a clear lack of evidence. The person may believe that either those nearby can perceive their thoughts or that they are being transmitted via mediums such as television, radio or the internet. Different people can experience thought broadcasting in different ways. Thought broadcasting is most commonly found among people who have a psychotic disorder, specifically schizophrenia.
This glossary covers terms found in the psychiatric literature; the word origins are primarily Greek, but there are also Latin, French, German, and English terms. Many of these terms refer to expressions dating from the early days of psychiatry in Europe.
Traumatic stress is a common term for reactive anxiety and depression, although it is not a medical term and is not included in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The experience of traumatic stress include subtypes of anxiety, depression and disturbance of conduct along with combinations of these symptoms. This may result from events that are less threatening and distressing than those that lead to post-traumatic stress disorder. The fifth edition of the DSM describes in a section titled "Trauma and Stress-Related Disorders" disinhibited social engagement disorder, reactive attachment disorder, acute stress disorder, adjustment disorder, and post-traumatic stress disorder.
Derealization is an alteration in the perception of the external world, causing those with the condition to perceive it as unreal, distant, distorted or falsified. Other symptoms include feeling as if one's environment is lacking in spontaneity, emotional coloring, and depth. It is a dissociative symptom that may appear in moments of severe stress.
Traumatic brain injury can cause a variety of complications, health effects that are not TBI themselves but that result from it. The risk of complications increases with the severity of the trauma; however even mild traumatic brain injury can result in disabilities that interfere with social interactions, employment, and everyday living. TBI can cause a variety of problems including physical, cognitive, emotional, and behavioral complications.
Childhood schizophrenia is similar in characteristics of schizophrenia that develops at a later age, but has an onset before the age of 13 years, and is more difficult to diagnose. Schizophrenia is characterized by positive symptoms that can include hallucinations, delusions, and disorganized speech; negative symptoms, such as blunted affect and avolition and apathy, and a number of cognitive impairments. Differential diagnosis is problematic since several other neurodevelopmental disorders, including autism spectrum disorder, language disorder, and attention deficit hyperactivity disorder, also have signs and symptoms similar to childhood-onset schizophrenia.
Pseudoneurotic schizophrenia is a postulated mental disorder categorized by the presence of two or more symptoms of mental illness such as anxiety, hysteria, and phobic or obsessive-compulsive neuroses. It is often acknowledged as a personality disorder. Patients generally display salient anxiety symptoms that disguise an underlying psychotic disorder.
References
- ↑ World Health Organization (2023). "MB25.3 Thought blocking". International Classification of Diseases, eleventh revision – ICD-11. Genova – icd.who.int.
- 1 2 3 Tani, Masayuki; Iwanami, Akira (October 2013). "[Disorder of train of thought in the elderly]". Nihon Rinsho. Japanese Journal of Clinical Medicine. 71 (10): 1793–1797. ISSN 0047-1852. PMID 24261209.
- ↑ Raymond Lake, C. (January 2008). "Disorders of thought are severe mood disorders: the selective attention defect in mania challenges the Kraepelinian dichotomy a review". Schizophrenia Bulletin. 34 (1): 109–117. doi:10.1093/schbul/sbm035. ISSN 0586-7614. PMC 2632389 . PMID 17515440.
- ↑ Nurcombe Barry, Ebert Michael H, "Chapter 4. The Psychiatric Interview" (Chapter). Ebert MH, Loosen PT, Nurcombe B, Leckman JF: CURRENT Diagnosis & Treatment: Psychiatry, p.2e: "AccessMedicine | the Psychiatric Interview: Introduction". Archived from the original on 2011-07-22. Retrieved 2010-07-20..
- ↑ "Blocking". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 28 February 2020.
- 1 2 3 Gelder, Mayou, Geddes (2005). Psychiatry. New York, NY; Oxford University Press Inc.
- ↑ Administration, Substance Abuse and Mental Health Services (June 2016). "Table 3.22, DSM-IV to DSM-5 Schizophrenia Comparison". www.ncbi.nlm.nih.gov. Retrieved 2020-11-10.
- ↑ Munir, Sadaf; Takov, Veronica (2020), "Generalized Anxiety Disorder", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28722900 , retrieved 2020-11-14
- ↑ Abood, Waleed; Bandyopadhyay, Susanta (2020), "Postictal Seizure State", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30252260 , retrieved 2020-11-14
- ↑ Treatment (US), Center for Substance Abuse (2014). "Exhibit 1.3-4, DSM-5 Diagnostic Criteria for PTSD". www.ncbi.nlm.nih.gov. Retrieved 2020-11-14.
- ↑ Hugo, Julie; Ganguli, Mary (August 2014). "Dementia and Cognitive Impairment: Epidemiology, Diagnosis, and Treatment". Clinics in Geriatric Medicine. 30 (3): 421–442. doi:10.1016/j.cger.2014.04.001. ISSN 0749-0690. PMC 4104432 . PMID 25037289.
- ↑ Shrimanker, Isha; Tadi, Prasanna; Sánchez-Manso, Juan Carlos (2020), "Parkinsonism", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31194381 , retrieved 2020-11-14