Related Research Articles
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that can develop because of exposure to a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.
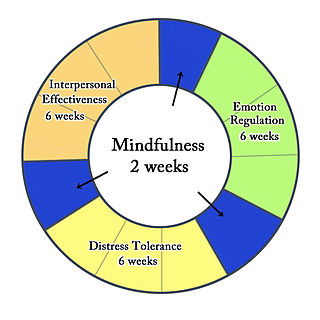
Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. There is evidence that DBT can be useful in treating mood disorders, suicidal ideation, and for change in behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies, and ultimately balance and synthesize them, in a manner comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.

Physical abuse is any intentional act causing injury or trauma to another person or animal by way of bodily contact. In most cases, children are the victims of physical abuse, but adults can also be victims, as in cases of domestic violence or workplace aggression. Alternative terms sometimes used include physical assault or physical violence, and may also include sexual abuse. Physical abuse may involve more than one abuser, and more than one victim.
Psychological trauma or mental trauma is an emotional response to a terrible event or series of events, such as accidents, rape or natural disasters. Reactions such as psychological shock and psychological denial are typical. Longer-term reactions include unpredictable emotions, flashbacks, difficulties with interpersonal relationships and sometimes physical symptoms including headaches or nausea.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.
Child psychopathology refers to the scientific study of mental disorders in children and adolescents. Oppositional defiant disorder, attention-deficit hyperactivity disorder, and autism spectrum disorder are examples of psychopathology that are typically first diagnosed during childhood. Mental health providers who work with children and adolescents are informed by research in developmental psychology, clinical child psychology, and family systems. Lists of child and adult mental disorders can be found in the International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10), published by the World Health Organization (WHO) and in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association (APA). In addition, the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood is used in assessing mental health and developmental disorders in children up to age five.
Developmental disability is a diverse group of chronic conditions that are due to mental or physical impairments that arise before adulthood. Developmental disabilities cause individuals living with them many difficulties in certain areas of life, especially in "language, mobility, learning, self-help, and independent living". Developmental disabilities can be detected early on and persist throughout an individual's lifespan. Developmental disability that affects all areas of a child's development is sometimes referred to as global developmental delay.
Dissociative disorders (DD) are conditions that involve disruptions or breakdowns of memory, awareness, identity, or perception. People with dissociative disorders use dissociation as a defense mechanism, pathologically and involuntarily. The individual suffers these dissociations to protect themselves. Some dissociative disorders are triggered by psychological trauma, but depersonalization-derealization disorder may be preceded only by stress, psychoactive substances, or no identifiable trigger at all.
Complex post-traumatic stress disorder is a psychological disorder that can develop in response to exposure to an extremely traumatic series of events in a context in which the individual perceives little or no chance of escape, and particularly where the exposure is prolonged or repetitive. In addition to the symptoms of post-traumatic stress disorder (PTSD), an individual with C-PTSD experiences emotional dysregulation, negative self-beliefs and feelings of shame, guilt or failure regarding the trauma, and interpersonal difficulties. C-PTSD relates to the trauma model of mental disorders and is associated with chronic sexual, psychological, and physical abuse or neglect, or chronic intimate partner violence, victims of kidnapping and hostage situations, indentured servants, victims of slavery and human trafficking, sweatshop workers, prisoners of war, concentration camp survivors, residential school survivors and prisoners kept in solitary confinement for a long period of time. It is most often directed at children and emotionally vulnerable adults, and whilst motivations behind such abuse vary, though mostly being predominantly malicious, it has also been shown that the motivations behind such abuse can occasionally be well-intentioned. Situations involving captivity/entrapment can lead to C-PTSD-like symptoms, which can include prolonged feelings of terror, worthlessness, helplessness, and deformation of one's identity and sense of self.
Emotional dysregulation is a term used in the mental health community that refers to emotional responses that are poorly modulated and do not lie within the accepted range of emotive response.
Childhood trauma is often described as serious adverse childhood experiences (ACEs). Children may go through a range of experiences that classify as psychological trauma; these might include neglect, abandonment, sexual abuse, emotional abuse, and physical abuse, witnessing abuse of a sibling or parent, or having a mentally ill parent. These events have profound psychological, physiological, and sociological impacts and can have negative, lasting effects on health and well-being such as unsocial behaviors, attention deficit hyperactivity disorder (ADHD), and sleep disturbances. Similarly, children with mothers who have experienced traumatic or stressful events during pregnancy can increase the child's risk of mental health disorders and other neurodevelopmental disorders. Kaiser Permanente and the Centers for Disease Control and Prevention's 1998 study on adverse childhood experiences determined that traumatic experiences during childhood are a root cause of many social, emotional, and cognitive impairments that lead to increased risk of unhealthy self-destructive behaviors, risk of violence or re-victimization, chronic health conditions, low life potential and premature mortality. As the number of adverse experiences increases, the risk of problems from childhood through adulthood also rises. Nearly 30 years of study following the initial study has confirmed this. Many states, health providers, and other groups now routinely screen parents and children for ACEs.
Prolonged exposure therapy (PE) is a form of behavior therapy and cognitive behavioral therapy designed to treat post-traumatic stress disorder. It is characterized by two main treatment procedures – imaginal and in vivo exposures. Imaginal exposure is repeated 'on-purpose' retelling of the trauma memory. In vivo exposure is gradually confronting situations, places, and things that are reminders of the trauma or feel dangerous. Additional procedures include processing of the trauma memory and breathing retraining.
PTSD, or post-traumatic stress disorder, is a psychiatric disorder characterized by intrusive thoughts and memories, dreams, or flashbacks of the event; avoidance of people, places, and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes, and persistent feelings of anger, guilt, or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep. PTSD is commonly treated with various types of psychotherapy, pharmacotherapy and/or biological interventions.
Neurological reparative therapy (NRT) is a new model of treatment synthesized from a compilation of literature and research on how to better the lives of individuals who suffer from a wide range of mental, emotional, and behavioral disturbances – particularly children and adolescents. Although the term "neurological reparative therapy" is new, the foundation of this model is not.
Transgenerational trauma, or intergenerational trauma, is the psychological effects that the collective trauma experienced by a group of people has on subsequent generations in that group. Collective trauma is the effect of psychological trauma experienced by communities and identity groups and carried as part of the group's collective memory and shared sense of identity. For example, collective trauma was experienced by descendants of the Atlantic Slave Trade, Segregation and Jim Crow Laws in the United States, Apartheid in South Africa, the Colonization of African countries, Jewish Holocaust survivors and other members of the Jewish community at the time, by the First Peoples of Canada during the Canadian Indian residential school system and in Australia. When this collective trauma affects subsequent generations, it is called transgenerational trauma. For example, if Jewish people experience extreme stress or practice survivalism out of fear of another Holocaust, despite being born after the end of the Holocaust, then they may be feeling transgenerational trauma.

Foster care in the modern sense was first introduced in the United Kingdom in 1853 when Reverend John Armistead removed children from a workhouse in Cheshire, and placed them with foster families. The local council was legally responsible for the children, and paid the foster parents a sum equal to the cost of maintaining the child in the workhouse.
Trauma focused cognitive behavioral therapy (TF-CBT) is an evidence-based psychotherapy or counselling that aims at addressing the needs of children and adolescents with post traumatic stress disorder (PTSD) and other difficulties related to traumatic life events. This treatment was developed and proposed by Drs. Anthony Mannarino, Judith Cohen, and Esther Deblinger in 2006. The goal of TF-CBT is to provide psychoeducation to both the child and non-offending caregivers, then help them identify, cope, and re-regulate maladaptive emotions, thoughts, and behaviors. Research has shown TF-CBT to be effective in treating childhood PTSD and with children who have experienced or witnessed traumatic events, including but not limited to physical or sexual victimization, child maltreatment, domestic violence, community violence, accidents, natural disasters, and war.
Early childhood trauma refers to various types of adversity and traumatic events experienced during the early years of a person's life. This is deemed the most critical developmental period in human life by psychologists. A critical period refers to a sensitive time during the early years of childhood in which children may be more vulnerable to be affected by environmental stimulation. These traumatic events can include serious sickness, natural disasters, family violence, sudden separation from a family member, being the victim of abuse, or suffering the loss of a loved one. Traumatic experiences in early childhood can result in severe consequences throughout adulthood, for instance developing post-traumatic stress disorder, depression, or anxiety. Negative childhood experiences can have a tremendous impact on future violence victimization and perpetration, and lifelong health and opportunity. However, not all children who are exposed to negative stimuli in early childhood will be affected severely in later life; some children come out unscathed after being faced with traumatic events, which is known as resilience. Many factors can account for the invulnerability displayed by certain children in response to adverse social conditions: gender, vulnerability, social support systems, and innate character traits. Much of the research in this area has referred to the Adverse Childhood Experiences Study (ACE) study.
Out-of-home placements are an alternative form of care when children must be removed from their homes. Children who are placed out of the home differ in the types and severity of maltreatment experienced compared to children who remain in the home. One-half to two-thirds of youth have experienced a traumatic event leading to increased awareness and growing literature on the impact of trauma on youth. The most common reasons for out-of-home placements are due to physical or sexual abuse, violence, and neglect. Youth who are at risk in their own homes for abuse, neglect, or maltreatment, as well as youth with severe emotional and behavior issues, are placed out of the home with extended family and friends, foster care, or in residential facilities. Out-of-home placements aim to provide children with safety and stability. This temporary, safe environment allows youth to have their physical, mental, moral, and social needs met. However, these youth are in a vulnerable position for experiencing repeated abuse and neglect.
Sexual trauma therapy is medical and psychological interventions provided to survivors of sexual violence aiming to treat their physical injuries and cope with mental trauma caused by the event. Examples of sexual violence include any acts of unwanted sexual actions like sexual harassment, groping, rape, and circulation of sexual content without consent.
References
- ↑ Diagnostic and Statistical Manual of Mental Disorders (Fourth ed.). American Psychiatric Association. 2000.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Saxe, GN; Ellis, BH; Kaplow, JB (2007). Collaborative Treatment of Traumatized Children and Teens: The Trauma Systems Therapy Approach. Guilford Press. ISBN 9781593853150.
- ↑ Saxe, GN; Ellis, BH; Fogler, J; Hansen, S; Sorkin, B (May 2005). "Comprehensive Care for Traumatized Children". Psychiatric Annals. 35 (5): 443–448. doi:10.3928/00485713-20050501-10.
- ↑ Hansen, S.; Saxe, G. (2009-02-17). "Trauma systems therapy: A replication of the model, integrating cognitive behavioral play therapy into child and family treatment". In Drewes, Athena A. (ed.). Blending play therapy with cognitive behavioral therapy: Evidence-based and other effective treatments and techniques . Hoboken, NJ: John Wiley & Sons. pp. 139–164. ISBN 9780470495520.
- ↑ TST Development Team. "TST Basics". Trauma Systems Therapy: Transforming the lives of traumatized children. Retrieved 2 October 2011.
- 1 2 Saxe, Glenn N. "TST Basics". Trauma Systems Blog. Retrieved 24 April 2012.
- ↑ "NCTSN Activities: NCTSN Indian County Child Trauma Center Sponsors American Indian Training". PsycEXTRA Dataset. 2004. doi:10.1037/e416582005-007 . Retrieved 2020-04-16.
- ↑ Hussey, David L.; Reed, Anne M.; Layman, Deborah L.; Pasiali, Varvara (2008-09-30). "Music Therapy and Complex Trauma: A Protocol for Developing Social Reciprocity". Residential Treatment for Children & Youth. 24 (1–2): 111–129. doi:10.1080/08865710802147547. ISSN 0886-571X. S2CID 144488049.
- 1 2 Saxe, Glenn N.; Heidi Ellis, B.; Fogler, Jason; Navalta, Carryl P. (2012). "Innovations in Practice: Preliminary evidence for effective family engagement in treatment for child traumatic stress-trauma systems therapy approach to preventing dropout". Child and Adolescent Mental Health. 1. 17 (1): 58–61. doi: 10.1111/j.1475-3588.2011.00626.x . PMID 32847314.