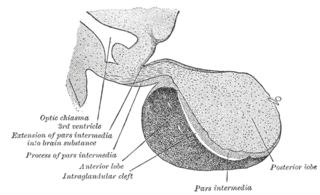
In vertebrate anatomy, the pituitary gland, or hypophysis, is an endocrine gland, about the size of a chickpea and weighing, on average, 0.5 grams (0.018 oz) in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain. The hypophysis rests upon the hypophyseal fossa of the sphenoid bone in the center of the middle cranial fossa and is surrounded by a small bony cavity covered by a dural fold.
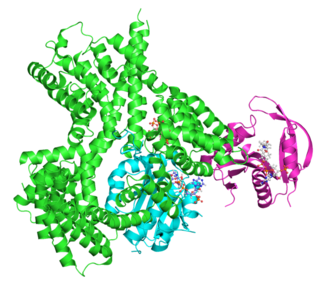
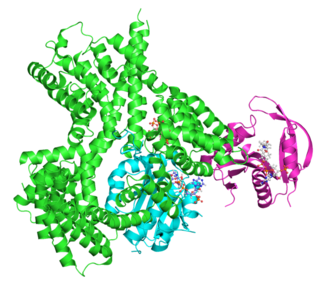
Adrenocorticotropic hormone is a polypeptide tropic hormone produced by and secreted by the anterior pituitary gland. It is also used as a medication and diagnostic agent. ACTH is an important component of the hypothalamic-pituitary-adrenal axis and is often produced in response to biological stress. Its principal effects are increased production and release of cortisol and androgens by the cortex and medulla of the adrenal gland, respectively. ACTH is also related to the circadian rhythm in many organisms.

Cushing's syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids such as cortisol. Signs and symptoms may include high blood pressure, abdominal obesity but with thin arms and legs, reddish stretch marks, a round red face, a fat lump between the shoulders, weak muscles, weak bones, acne, and fragile skin that heals poorly. Women may have more hair and irregular menstruation. Occasionally there may be changes in mood, headaches, and a chronic feeling of tiredness.

Stress, either physiological, biological or psychological, is an organism's response to a stressor such as an environmental condition. Stress is the body's method of reacting to a condition such as a threat, challenge or physical and psychological barrier. There are two hormones that an individual produces during a stressful situation, these are well known as adrenaline and cortisol. There are two kinds of stress hormone levels. Resting (basal) cortisol levels are normal everyday quantities that are essential for standard functioning. Reactive cortisol levels are increases in cortisol in response to stressors. Stimuli that alter an organism's environment are responded to by multiple systems in the body. In humans and most mammals, the autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are the two major systems that respond to stress.

The hypothalamic–pituitary–adrenal axis is a complex set of direct influences and feedback interactions among three components: the hypothalamus, the pituitary gland, and the adrenal glands. These organs and their interactions constitute the HPA axis.
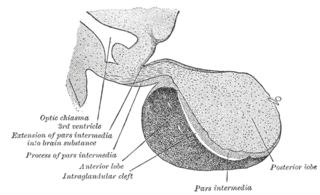
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis). The anterior pituitary regulates several physiological processes, including stress, growth, reproduction, and lactation. Proper functioning of the anterior pituitary and of the organs it regulates can often be ascertained via blood tests that measure hormone levels.

Cortisol is a steroid hormone, in the glucocorticoid class of hormones. When used as a medication, it is known as hydrocortisone.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal gland normally secretes glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. An adrenal crisis may occur if the body is subjected to stress, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Corticotropes are basophilic cells in the anterior pituitary that produce pro-opiomelanocortin (POMC) which undergoes cleavage to adrenocorticotropin (ACTH), β-lipotropin (β-LPH), and melanocyte-stimulating hormone (MSH). These cells are stimulated by corticotropin releasing hormone (CRH) and make up 15–20% of the cells in the anterior pituitary. The release of ACTH from the corticotropic cells is controlled by CRH, which is formed in the cell bodies of parvocellular neurosecretory cells within the paraventricular nucleus of the hypothalamus and passes to the corticotropes in the anterior pituitary via the hypophyseal portal system. Adrenocorticotropin hormone stimulates the adrenal cortex to release glucocorticoids and plays an important role in the stress response.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.
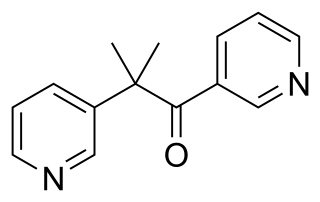
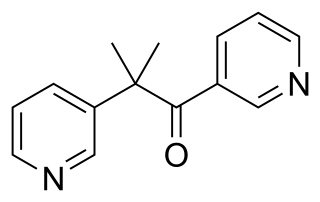
Metyrapone, sold under the brand name Metopirone, is a medication which is used in the diagnosis of adrenal insufficiency and occasionally in the treatment of Cushing's syndrome (hypercortisolism).
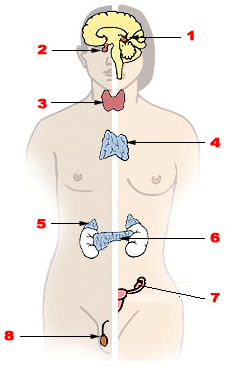
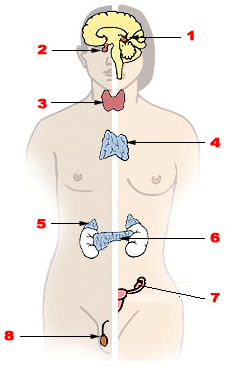
Endocrine glands are ductless glands of the endocrine system that secrete their products, hormones, directly into the blood. The major glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testes, thyroid gland, parathyroid gland, hypothalamus and adrenal glands. The hypothalamus and pituitary glands are neuroendocrine organs.
Human bonding is the process of development of a close, interpersonal relationship between two or more people. It most commonly takes place between family members or friends, but can also develop among groups, such as sporting teams and whenever people spend time together. Bonding is a mutual, interactive process, and is different from simple liking. It is the process of nurturing social connection.
In humans and other animals, the adrenocortical hormones are hormones produced by the adrenal cortex, the outer region of the adrenal gland. These polycyclic steroid hormones have a variety of roles that are crucial for the body’s response to stress, and they also regulate other functions in the body. Threats to homeostasis, such as injury, chemical imbalances, infection, or psychological stress, can initiate a stress response. Examples of adrenocortical hormones that are involved in the stress response are aldosterone and cortisol. These hormones also function in regulating the conservation of water by the kidneys and glucose metabolism, respectively.
An insulin tolerance test (ITT) is a medical diagnostic procedure during which insulin is injected into a patient's vein, after which blood glucose is measured at regular intervals. This procedure is performed to assess pituitary function, adrenal function, insulin sensitivity, and sometimes for other purposes. An ITT is usually ordered and interpreted by endocrinologists.
The ACTH test is a medical test usually requested and interpreted by endocrinologists to assess the functioning of the adrenal glands' stress response by measuring the adrenal response to adrenocorticotropic hormone or another corticotropic agent such as tetracosactide or alsactide (Synchrodyn). ACTH is a hormone produced in the anterior pituitary gland that stimulates the adrenal glands to release cortisol, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), and aldosterone.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.

The cortisol awakening response (CAR) is an increase between 38% and 75% in cortisol levels peaking 30–45 minutes after awakening in the morning in some people. This rise is superimposed upon the late-night rise in cortisol which occurs before awakening. While its purpose is uncertain, it may be linked to the hippocampus' preparation of the hypothalamic-pituitary-adrenal axis (HPA) in order to face anticipated stress.

Social stress is stress that stems from one's relationships with others and from the social environment in general. Based on the appraisal theory of emotion, stress arises when a person evaluates a situation as personally relevant and perceives that they do not have the resources to cope or handle the specific situation. The activation of social stress does not necessarily have to occur linked to a specific event, the mere idea that the event may occur could trigger it. This means that any element that takes a subject out of their personal and intimate environment could become a stressful experience. Situation that makes them socially incompetent individuals.
Maternal fetal stress transfer describes the physiological phenomenon by which psychosocial stress experienced by a mother during her pregnancy can be transferred to the fetus. Psychosocial stress describes the brain's physiological response to perceived social threat. Because of a link in blood supply between a mother and fetus, it has been found that stress can leave lasting effects on a developing fetus, even before a child is born. According to recent studies, these effects are mainly the result of two particular stress biomarkers circulating in the maternal blood supply: cortisol and catecholamines.