Related Research Articles
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland, or organ function depending on which nerves are affected; in other words, neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

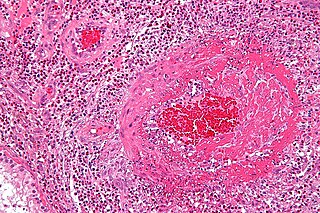
Vasculitis is a group of disorders that destroy blood vessels by inflammation. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis. Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.

Granulomatosis with polyangiitis (GPA), previously known as Wegener's granulomatosis (WG), is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy).

Polyarteritis nodosa (PAN) is a systemic necrotizing inflammation of blood vessels (vasculitis) affecting medium-sized muscular arteries, typically involving the arteries of the kidneys and other internal organs but generally sparing the lungs' circulation. Small aneurysms are strung like the beads of a rosary, therefore making this "rosary sign" an important diagnostic feature of the vasculitis. PAN is sometimes associated with infection by the hepatitis B or hepatitis C virus. The condition may be present in infants.
Neuropathic pain is pain caused by damage or disease affecting the somatosensory system. Neuropathic pain may be associated with abnormal sensations called dysesthesia or pain from normally non-painful stimuli (allodynia). It may have continuous and/or episodic (paroxysmal) components. The latter resemble stabbings or electric shocks. Common qualities include burning or coldness, "pins and needles" sensations, numbness and itching.
Microscopic polyangiitis is an ill-defined autoimmune disease characterized by a systemic, pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of necrotizing granulomatous inflammation.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
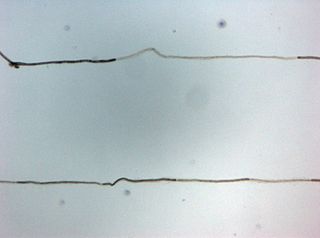
Small fiber peripheral neuropathy is a type of peripheral neuropathy that occurs from damage to the small unmyelinated and myelinated peripheral nerve fibers. These fibers, categorized as C fibers and small Aδ fibers, are present in skin, peripheral nerves, and organs. The role of these nerves is to innervate the skin and help control autonomic function. It is estimated that 15–20 million people in the United States have some form of peripheral neuropathy.
An overlap syndrome is a medical condition which shares features of at least two more widely recognised disorders. Examples of overlap syndromes can be found in many medical specialties such as overlapping connective tissue disorders in rheumatology, and overlapping genetic disorders in cardiology.
Vasa nervorum are small arteries that provide blood supply to peripheral nerves, specifically to the interior parts of nerves, and their coverings.
Necrotizing vasculitis, also called systemic necrotizing vasculitus, is a category of vasculitis, comprising vasculitides that present with necrosis.

A diabetic foot is any pathology that results directly from peripheral arterial disease (PAD) and/or sensory neuropathy affecting the feet in diabetes mellitus; it is a long-term complication of diabetes mellitus. Presence of several characteristic diabetic foot pathologies such as infection, diabetic foot ulcer and neuropathic osteoarthropathy is called diabetic foot syndrome. The resulting bone deformity is known as Charcot foot.
Microvasculitis refers to a range of diseases or presentations associated with a disease, where there is inflammation of small blood vessels:
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.

Quantitative sensory testing (QST) is a panel of diagnostic tests used to assess somatosensory function, in the context of research and as a supplemental tool in the diagnosis of somatosensory disorders, including pain insensitivity, painless and painful neuropathy. The panel of tests examine a broad range of different sensations, including hot, cold, touch, vibration. It has both positive and negative tests. QST reflects a formalisation of existing neurological tests into a standardised battery designed to detect subtle changes in sensory function. Large datasets representing normal responses to sensory tests have been established to quantitate deviation from the mean and allow comparison with normal patients. It is thought that a detailed evaluation of somatosensory function may be useful in identifying subtypes of pain and as a potential tool to identify asymptomatic neuropathy, which may represent up to 50% of total people with neuropathy. In clinical use, it is often combined with other tests such as clinical electrophysiology. In research settings it is increasingly applied in combination with advanced imaging such as fMRI, epidermis "nerve" biopsies and microneurography to classify subtypes of painful disorders.
Electrochemical skin conductance (ESC) is an objective, non-invasive and quantitative electrophysiological measure. It is based on reverse iontophoresis and (multiple) steady chronoamperometry.
References
- 1 2 3 4 Graf, Jonathan; Imboden, John (January 2019). "Vasculitis and peripheral neuropathy". Current Opinion in Rheumatology. 31 (1): 40–45. doi:10.1097/BOR.0000000000000559. ISSN 1040-8711. PMID 30461543. S2CID 53943955.
- 1 2 3 4 5 Collins, Michael P.; Dyck, P. James B.; Hadden, Robert D.M. (October 2019). "Update on classification, epidemiology, clinical phenotype and imaging of the nonsystemic vasculitic neuropathies". Current Opinion in Neurology. 32 (5): 684–695. doi:10.1097/WCO.0000000000000727. ISSN 1350-7540. PMID 31313704. S2CID 197423473.
- 1 2 3 4 5 6 7 8 Collins, Michael P.; Hadden, Robert D. (May 2017). "The nonsystemic vasculitic neuropathies". Nature Reviews Neurology. 13 (5): 302–316. doi: 10.1038/nrneurol.2017.42 . ISSN 1759-4758. PMID 28447661.