Related Research Articles

Dementia is the general name for a decline in cognitive abilities that impacts a person's ability to perform everyday activities. This typically involves problems with memory, thinking, and behavior. Aside from memory impairment and a disruption in thought patterns, the most common symptoms include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, caregivers, and on social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than what is caused by normal aging.

Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia, rigidity, and postural instability. These are the four motor symptoms found in Parkinson's disease (PD) – after which it is named – dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.
Vascular dementia (VaD) is dementia caused by problems in the blood supply to the brain, resulting from a cerebrovascular disease. Restricted blood supply (ischemia) leads to cell and tissue death in the affected region, known as an infarct. The three types of vascular dementia are subcortical vascular dementia, multi-infarct dementia, and stroke related dementia. Subcortical vascular dementia is brought about by damage to the small blood vessels in the brain. Multi-infarct dementia is brought about by a series of mini-strokes where many regions have been affected. The third type is stroke related where more serious damage may result. Such damage leads to varying levels of cognitive decline. When caused by mini-strokes, the decline in cognition is gradual. When due to a stroke, the cognitive decline can be traced back to the event.
Normal pressure hydrocephalus (NPH), also called malresorptive hydrocephalus, is a form of communicating hydrocephalus in which excess cerebrospinal fluid (CSF) builds up in the ventricles, leading to normal or slightly elevated cerebrospinal fluid pressure. The fluid build-up causes the ventricles to enlarge and the pressure inside the head to increase, compressing surrounding brain tissue and leading to neurological complications. Although the cause of idiopathicNPH remains unclear, it has been associated with various co-morbidities including hypertension, diabetes mellitus, Alzheimer's disease, and hyperlipidemia. Causes of secondary NPH include trauma, hemorrhage, or infection. The disease presents in a classic triad of symptoms, which are memory impairment, urinary frequency, and balance problems/gait deviations. The disease was first described by Salomón Hakim and Raymond Adams in 1965.
Semantic dementia (SD), also known as semantic variant primary progressive aphasia (svPPA), is a progressive neurodegenerative disorder characterized by loss of semantic memory in both the verbal and non-verbal domains. However, the most common presenting symptoms are in the verbal domain. Semantic dementia is a disorder of semantic memory that causes patients to lose the ability to match words or images to their meanings. However, it is fairly rare for patients with semantic dementia to develop category specific impairments, though there have been documented cases of it occurring. Typically, a more generalized semantic impairment results from dimmed semantic representations in the brain.
Progressive nonfluent aphasia (PNFA) is one of three clinical syndromes associated with frontotemporal lobar degeneration. PNFA has an insidious onset of language deficits over time as opposed to other stroke-based aphasias, which occur acutely following trauma to the brain. The specific degeneration of the frontal and temporal lobes in PNFA creates hallmark language deficits differentiating this disorder from other Alzheimer-type disorders by the initial absence of other cognitive and memory deficits. This disorder commonly has a primary effect on the left hemisphere, causing the symptomatic display of expressive language deficits and sometimes may disrupt receptive abilities in comprehending grammatically complex language.
J. William Langston is the founder and chief scientific officer, movement disorder specialist, and chief executive officer of the Parkinson's Institute and Clinical Center in Sunnyvale, California, the founding member of the Scientific Advisory Board for the Michael J. Fox Foundation and the Co-Editor-in-Chief of the Journal of Parkinson's Disease. He is a graduate of the University of Missouri School of Medicine. Langston was formerly a faculty member at Stanford University and Chairman of Neurology at Santa Clara Valley Medical Center in San Jose, California. Langston has authored or co-authored some 360 peer-reviewed articles in the field of neurology, most of which are on Parkinson's disease and related disorders. Langston gained national and international recognition in 1982 for the discovery of the link between a "synthetic heroin" contaminant (MPTP) and parkinsonism.

Apolipoprotein E (Apo-E) is a protein involved in the metabolism of fats in the body of mammals. A subtype is implicated in the Alzheimer's disease and cardiovascular diseases. It is encoded in humans by the gene APOE.
Cognitive reserve is the mind's and brain's resistance to damage of the brain. The mind's resilience is evaluated behaviorally, whereas the neuropathological damage is evaluated histologically, although damage may be estimated using blood-based markers and imaging methods. There are two models that can be used when exploring the concept of "reserve": brain reserve and cognitive reserve. These terms, albeit often used interchangeably in the literature, provide a useful way of discussing the models. Using a computer analogy, brain reserve can be seen as hardware and cognitive reserve as software. All these factors are currently believed to contribute to global reserve. Cognitive reserve is commonly used to refer to both brain and cognitive reserves in the literature.
The prevention of dementia involves reducing the number of risk factors for the development of dementia, and is a global health priority needing a global response. Initiatives include the establishment of the International Research Network on Dementia Prevention (IRNDP) which aims to link researchers in this field globally, and the establishment of the Global Dementia Observatory a web-based data knowledge and exchange platform, which will collate and disseminate key dementia data from members states. Although there is no cure for dementia, it is well established that modifiable risk factors influence both the likelihood of developing dementia and the age at which it is developed. Dementia can be prevented by reducing the risk factors for vascular disease such as diabetes, high blood pressure, obesity, smoking, physical inactivity and depression. A study concluded that more than a third of dementia cases are theoretically preventable. Among older adults both an unfavorable lifestyle and high genetic risk are independently associated with higher dementia risk. A favorable lifestyle is associated with a lower dementia risk, regardless of genetic risk. In 2020, a study identified 12 modifiable lifestyle factors, and the early treatment of acquired hearing loss was estimated as the most significant of these factors, potentially preventing up to 9% of dementia cases.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens, and is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.
Subcortical dementias includes those diseases which predominantly affects the basal ganglia along with features of cognitive decline.
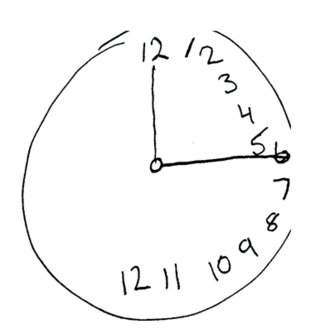
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.

Rivastigmine is a cholinesterase inhibitor used for the treatment of mild to moderate Alzheimer's disease. The drug can be administered orally or via a transdermal patch; the latter form reduces the prevalence of side effects, which typically include nausea and vomiting.
Parkinson's disease dementia (PDD) is dementia that is associated with Parkinson's disease (PD). Together with dementia with Lewy bodies (DLB), it is one of the Lewy body dementias characterized by abnormal deposits of Lewy bodies in the brain.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.

Gladys Elena Maestre is a neuroscientist from Venezuela who is a professor at the University of Texas Rio Grande Valley School of Medicine. She is known for her work on Alzheimer's disease and other forms of dementia.
Nicole Schupf is an American epidemiologist and neuroscientist who is Professor of Epidemiology in Neurology, Psychiatry, the Gertrude H. Sergievsky Center, and the Taub Institute for Research on Alzheimer's Disease and the Aging Brain, Columbia University Faculty of Medicine. She studies aging and Alzheimer's disease in individuals with Down syndrome.
Andrew E. Budson is an American neurologist, academic and researcher. He is a Professor of Neurology at Boston University School of Medicine, Lecturer in Neurology at Harvard Medical School, Chief of Cognitive and Behavioral Neurology and Associate Chief of Staff for Education at the Veterans Affairs (VA) Boston Healthcare System, where he also serves as a Director of the Center for Translational Cognitive Neuroscience. He is Associate Director and Outreach, Recruitment, and Engagement Core Leader at the Boston University Alzheimer's Disease Research Center.
David A Bennett is a neurologist, Director of the Rush Alzheimer's Disease Center (RADC), and the Robert C Borwell Professor of Neurology at Rush University Medical Center.Bennett is also Visiting Professor, Instituto de Assistencia Medica ao Servidor Publico Estadual (IAMSPE), São Paulo, Brazil.
References
- ↑ "Bio". 14 October 2020.
- ↑ Stern, Y. (2002). "What is cognitive reserve? Theory and research application of the reserve concept". Journal of the International Neuropsychological Society. 8 (3): 448–460. doi:10.1017/s1355617702813248. PMID 11939702. S2CID 9902333.
- ↑ "Journal of Alzheimer's Disease".
- ↑ Heidi Godman (December 21, 2018). "Can I Bank Cognition Now for Old Age?". U.S. News & World Report .
- ↑ "Five myths about Alzheimer's disease". June 15, 2018.
- ↑ Cecilia Pessoa Gingerich (April 17, 2018). "Physicians with Alzheimer's: What Happens When a Doctor Forgets?".
- ↑ Stern, Y.; Alexander, GE; Prohovnik, I.; Mayeux, R. (1992). "Inverse relationship between education and parietotemporal perfusion deficit in Alzheimer's disease". Annals of Neurology. 32 (3): 371–375. doi:10.1002/ana.410320311. PMID 1416806. S2CID 20777087.
- ↑ Stern, Y.; Gurland, B.; Tatemichi, TK; Tang, MX; Wilder, D.; Mayeux, R. (1994). "Influence of education and occupation on the incidence of Alzheimer's disease". Journal of the American Medical Association. 271 (13): 1004–1010. doi:10.1001/jama.1994.03510370056032. PMID 8139057.
- ↑ Scarmeas, N.; Levy, G.; Tang, MX; Manly, J.; Stern, Y. (2001). "Influence of leisure activity on the incidence of Alzheimer's disease". Neurology. 57 (12): 2236–2242. doi:10.1212/wnl.57.12.2236. PMC 3025284 . PMID 11756603.
- ↑ Stern, Y.; Albert, S.; Tang, MX; Tsai, WY (1999). "Rate of memory decline in AD is related to education and occupation: Cognitive reserve?". Neurology. 53 (9): 1942–1957. doi:10.1212/wnl.53.9.1942. PMID 10599762. S2CID 5676450.
- ↑ Stern, Y. (2009). "Cognitive reserve". Neuropsychologia. 47 (10): 2015–2028. doi:10.1016/j.neuropsychologia.2009.03.004. PMC 2739591 . PMID 19467352.
- ↑ Stern, Yaakov (2006). Cognitive Reserve: Theory and Applications (1st ed.). New York and London: Taylor & Francis. ISBN 9781138006263.
- ↑ Stern, Y.; Mayeux, R.; Rosen, J.; Ilson, J. (1983). "Perceptual motor dysfunction in Parkinson's disease: a deficit in sequential and predictive voluntary movement". Journal of Neurology, Neurosurgery, and Psychiatry. 46 (2): 145–151. doi:10.1136/jnnp.46.2.145. PMC 1027297 . PMID 6842218.
- ↑ Stern, Y.; Langston, JW (1985). "Intellectual changes in patients with MPTP-induced parkinsonism". Neurology. 35 (10): 1506–1509. doi:10.1212/wnl.35.10.1506. PMID 3875807. S2CID 7914649.
- ↑ Stern, Y.; Tang, MX; Albert, MS (1997). "Predicting time to nursing home care and death in individuals with Alzheimer disease". Journal of the American Medical Association. 277 (10): 806–812. doi:10.1001/jama.277.10.806. PMID 9052710.
- ↑ Stern, Y.; Habeck, C.; Steffener, J. (2014). "The Reference Ability Neural Network Study: motivation, design, and initial feasibility analyses". NeuroImage. 103: 139–151. doi:10.1016/j.neuroimage.2014.09.029. PMC 4312259 . PMID 25245813.