Related Research Articles
A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also means local hypoxia in a given part of a body sometimes resulting from constriction. Ischemia comprises not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed so that it is adequate.
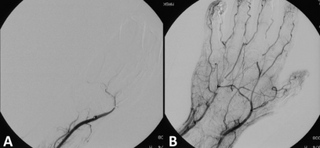
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.

The thiazolidinediones, abbreviated as TZD, also known as glitazones after the prototypical drug ciglitazone, are a class of heterocyclic compounds consisting of a five-membered C3NS ring. The term usually refers to a family of drugs used in the treatment of diabetes mellitus type 2 that were introduced in the late 1990s.

A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.

Amaurosis fugax is a painless temporary loss of vision in one or both eyes.
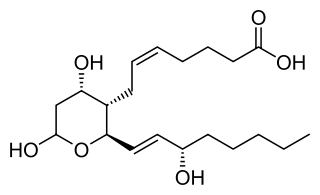
Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

Transient global amnesia (TGA) is a neurological disorder whose key defining characteristic is a temporary but almost total disruption of short-term memory with a range of problems accessing older memories. A person in a state of TGA exhibits no other signs of impaired cognitive functioning but recalls only the last few moments of consciousness, as well as possibly a few deeply encoded facts of the individual's past, such as their childhood, family, or home perhaps.
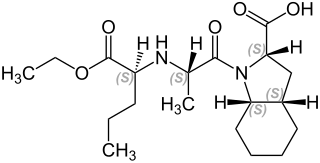
Perindopril is a medication used to treat high blood pressure, heart failure, or stable coronary artery disease.
The CHADS2 score and its updated version, the CHA2DS2-VASc score, are clinical prediction rules for estimating the risk of stroke in people with non-rheumatic atrial fibrillation (AF), a common and serious heart arrhythmia associated with thromboembolic stroke. Such a score is used to determine whether or not treatment is required with anticoagulation therapy or antiplatelet therapy, since AF can cause stasis of blood in the upper heart chambers, leading to the formation of a mural thrombus that can dislodge into the blood flow, reach the brain, cut off supply to the brain, and cause a stroke.
The management of atrial fibrillation (AF) is focused on preventing temporary circulatory instability, stroke and other ischemic events. Control of heart rate and rhythm are principally used to achieve the former, while anticoagulation may be employed to decrease the risk of stroke. Within the context of stroke, the discipline may be referred to as stroke prevention in atrial fibrillation (SPAF). In emergencies, when circulatory collapse is imminent due to uncontrolled rapid heart rate, immediate cardioversion may be indicated.
The Framingham Risk Score is a sex-specific algorithm used to estimate the 10-year cardiovascular risk of an individual. The Framingham Risk Score was first developed based on data obtained from the Framingham Heart Study, to estimate the 10-year risk of developing coronary heart disease. In order to assess the 10-year cardiovascular disease risk, cerebrovascular events, peripheral artery disease and heart failure were subsequently added as disease outcomes for the 2008 Framingham Risk Score, on top of coronary heart disease.
A silent stroke is a stroke that does not have any outward symptoms associated with stroke, and the patient is typically unaware they have suffered a stroke. Despite not causing identifiable symptoms, a silent stroke still causes damage to the brain and places the patient at increased risk for both transient ischemic attack and major stroke in the future. In a broad study in 1998, more than 11 million people were estimated to have experienced a stroke in the United States. Approximately 770,000 of these strokes were symptomatic and 11 million were first-ever silent MRI infarcts or hemorrhages. Silent strokes typically cause lesions which are detected via the use of neuroimaging such as MRI. The risk of silent stroke increases with age but may also affect younger adults. Women appear to be at increased risk for silent stroke, with hypertension and current cigarette smoking being amongst the predisposing factors.

The Caerphilly Heart Disease Study, also known as the Caerphilly Prospective Study (CaPS), is an epidemiological prospective cohort, set up in 1979 in a representative population sample drawn from Caerphilly, a typical small town in South Wales, UK.
Remote ischemic conditioning (RIC) is an experimental medical procedure that aims to reduce the severity of ischaemic injury to an organ such as the heart or the brain, most commonly in the situation of a heart attack or a stroke, or during procedures such as heart surgery when the heart may temporary suffer ischaemia during the operation, by triggering the body's natural protection against tissue injury. Although noted to have some benefits in experimental models in animals, this is still an experimental procedure in humans and initial evidence from small studies have not been replicated in larger clinical trials. Successive clinical trials have failed to identify evidence supporting a protective role in humans.
Embolic stroke of undetermined source (ESUS) is a type of ischemic stroke with an unknown origin, defined as a non-lacunar brain infarct without proximal arterial stenosis or cardioembolic sources. As such, it forms a subset of cryptogenic stroke, which is part of the TOAST-classification. The following diagnostic criteria define an ESUS:
References
- 1 2 3 4 Gommans J, Barber PA, Fink J (April 2009). "Preventing strokes: the assessment and management of people with transient ischaemic attack" (PDF). N. Z. Med. J. 122 (1293): 3556. PMID 19448791. Archived from the original (PDF) on 2010-06-05.
- ↑ Galvin R, Geraghty C, Motterlini N, Dimitrov BD, Fahey T (August 2011). "Prognostic value of the ABCD² clinical prediction rule: a systematic review and meta-analysis". Fam Pract. 28 (4): 366–76. doi: 10.1093/fampra/cmr008 . PMID 21486940.
- 1 2 Wardlaw, JM; Brazzelli, M; Chappell, FM; Miranda, H; Shuler, K; Sandercock, PA; Dennis, MS (28 July 2015). "ABCD2 score and secondary stroke prevention: meta-analysis and effect per 1,000 patients triaged". Neurology. 85 (4): 373–80. doi:10.1212/wnl.0000000000001780. PMC 4520819 . PMID 26136519.
- ↑ Giles MF, Rothwell PM (2010). "Systematic review and pooled analysis of published and unpublished validations of the ABCD and ABCD2 transient ischemic attack risk scores". Stroke. 41 (4): 667–73. doi: 10.1161/STROKEAHA.109.571174 . PMID 20185786.
- ↑ Rothwell PM, Giles MF, Flossmann E, et al. (2005). "A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack". Lancet. 366 (9479): 29–36. doi:10.1016/S0140-6736(05)66702-5. PMID 15993230. S2CID 20859717.
- ↑ Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. (January 2007). "Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack". Lancet. 369 (9558): 283–92. doi:10.1016/S0140-6736(07)60150-0. PMID 17258668. S2CID 9510865.
- ↑ Perry JJ, Sharma M, Sivilotti ML, Sutherland J, Symington C, Worster A, Émond M, Stotts G, Jin AY, Oczkowski WJ, Sahlas DJ, Murray HE, MacKey A, Verreault S, Wells GA, Stiell IG (2011). "Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack". Canadian Medical Association Journal. 183 (10): 1137–45. doi:10.1503/cmaj.101668. PMC 3134721 . PMID 21646462.