Related Research Articles
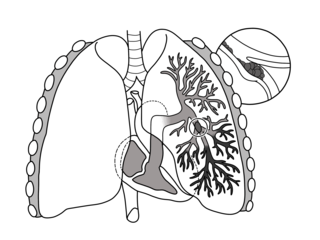
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

A prediction or forecast is a statement about a future event or about future data. Predictions are often, but not always, based upon experience or knowledge of forecasters. There is no universal agreement about the exact difference between "prediction" and "estimation"; different authors and disciplines ascribe different connotations.

In a physical examination, medical examination, clinical examination, or medical checkup, a medical practitioner examines a patient for any possible medical signs or symptoms of a medical condition. It generally consists of a series of questions about the patient's medical history followed by an examination based on the reported symptoms. Together, the medical history and the physical examination help to determine a diagnosis and devise the treatment plan. These data then become part of the medical record.
In medical or research imaging, an incidental imaging finding is an unanticipated finding which is not related to the original diagnostic inquiry. As with other types of incidental medical findings, they may represent a diagnostic, ethical, and philosophical dilemma because their significance is unclear. While some coincidental findings may lead to beneficial diagnoses, others may lead to overdiagnosis that results in unnecessary testing and treatment, sometimes called the "cascade effect".
A medical error is a preventable adverse effect of care ("iatrogenesis"), whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment.
A serious adverse event (SAE) in human drug trials is defined as any untoward medical occurrence that at any dose
- Results in death
- Is life-threatening
- Requires inpatient hospitalization or causes prolongation of existing hospitalization
- Results in persistent or significant disability/incapacity
- May have caused a congenital anomaly/birth defect
- Requires intervention to prevent permanent impairment or damage
The pneumonia severity index (PSI) or PORT Score is a clinical prediction rule that medical practitioners can use to calculate the probability of morbidity and mortality among patients with community acquired pneumonia.

Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by a bacterial infection, rather than a virus.
Brainerd diarrhea is a sudden-onset watery, explosive diarrhea that lasts for months and does not respond to antibiotics; the cause of Brainerd diarrhea is unknown. Brainerd diarrhea was first described in Brainerd, Minnesota in 1983. It has been associated with the consumption of raw milk and untreated water. Of the ten outbreaks reported since 1983, nine have been in the U.S. The characteristics of each outbreak have been similar to that caused by an infectious agent. Although a comparatively large outbreak occurred in 1996 in Fannin County, Texas, the largest outbreak was the original one in Brainerd, MN. There have been no secondary cases reported in any of the outbreaks, suggesting that the causative agent cannot be passed from person to person, but boiling water appears to inactivate the Brainerd agent. Although there is no treatment available, the disease does appear to resolve itself, although this process takes months if not years.
In biostatistics, spectrum bias refers to the phenomenon that the performance of a diagnostic test may vary in different clinical settings because each setting has a different mix of patients. Because the performance may be dependent on the mix of patients, performance at one clinic may not be predictive of performance at another clinic. These differences are interpreted as a kind of bias. Mathematically, the spectrum bias is a sampling bias and not a traditional statistical bias; this has led some authors to refer to the phenomenon as spectrum effects, whilst others maintain it is a bias if the true performance of the test differs from that which is 'expected'. Usually the performance of a diagnostic test is measured in terms of its sensitivity and specificity and it is changes in these that are considered when referring to spectrum bias. However, other performance measures such as the likelihood ratios may also be affected by spectrum bias.
Allen Caruthers Steere is an American rheumatologist. He is a professor of rheumatology at Harvard University and previously at Tufts University and Yale University. Steere and his mentor, Stephen Malawista of Yale University, are credited with discovering and naming Lyme disease, and he has published almost 300 scholarly articles on Lyme disease during his more than 40 years of studies of this infection. At a ceremony in Hartford, Connecticut in 1998, Governor John G. Rowland declared September 24 to be "Allen C. Steere Day".
The United States Preventive Services Task Force (USPSTF) is "an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services". The task force, a volunteer panel of primary care clinicians with methodology experience including epidemiology, biostatistics, health services research, decision sciences, and health economics, is funded, staffed, and appointed by the U.S. Department of Health and Human Services' Agency for Healthcare Research and Quality.
George P. Canellos is an American oncologist and cancer researcher. His research career spans many decades, as well as several areas of therapeutic agents for the treatment of malignant diseases. He is perhaps most known for his work with Vincent T. DeVita in which he developed the combination chemotherapy CMF, which was one of the first combination therapies for breast cancer. The two also collaborated to create the MOPP regimen for Hodgkin's lymphoma.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.
David M. Eddy is an American physician, mathematician, and healthcare analyst who has done seminal work in mathematical modeling of diseases, clinical practice guidelines, and evidence-based medicine. Four highlights of his career have been summarized by the Institute of Medicine of the National Academy of Sciences: "more than 25 years ago, Eddy wrote the seminal paper on the role of guidelines in medical decision-making, the first Markov model applied to clinical problems, and the original criteria for coverage decisions; he was the first to use and publish the term 'evidence-based'."
Isabelle Boutron is a professor of epidemiology at the Université Paris Cité and head of the INSERM- METHODS team within the Centre of Research in Epidemiology and Statistics (CRESS). She was originally trained in rheumatology and later switched to a career in epidemiology and public health. She is also deputy director of the French EQUATOR Centre, member of the SPIRIT-CONSORT executive committee, director of Cochrane France and co-convenor of the Bias Methods group of the Cochrane Collaboration.

Cynthia Mulrow is an American physician and scholar from Edinburg, Texas. She has regularly contributed academic research on many topics to the medical community. Her academic work mainly focuses on systematic reviews and evidence reports, research methodology, and chronic medical conditions.

Andrew S. Levey is an American nephrologist who transformed chronic kidney disease (CKD) clinical practice, research, and public health by developing equations to estimate glomerular filtration rate (GFR), and leading the global standardization of CKD definition and staging.
Harlan M. Krumholz, MD, SM is an American cardiologist, leading research scientist, and the Harold H. Hines, Jr. Professor of Medicine at Yale School of Medicine, where he has been on faculty since 1992. A pioneer in the development of the field of outcomes research, his groundbreaking contributions to science have directly led to improvements in healthcare outcomes for patients and populations. He is an international expert in the science to evaluate and improve the quality and efficiency of care, reduce disparities, improve integrity in medical research, promote better health policies and regulations, and promote patient-centeredness in research and clinical care. He is the founder and director of the Yale New Haven Hospital Center for Outcomes Research and Evaluation.
The Wells score is a clinical prediction rule used to classify patients suspected of having pulmonary embolism (PE) into risk groups by quantifying the pre-test probability. It is different than Wells score for DVT. It was originally described by Wells et al. in 1998, using their experience from creating Wells score for DVT in 1995. Today, there are multiple versions of the rule, which may lead to ambiguity.
References
- ↑ McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Stiell IG, Richardson WS (2000). "Users' guides to the medical literature: XXII: how to use articles about clinical decision rules. Evidence-Based Medicine Working Group". JAMA. 284 (1): 79–84. doi:10.1001/jama.284.1.79. PMID 10872017.
- ↑ Friedmann PD, Brett AS, Mayo-Smith MF (1996). "Differences in generalists' and cardiologists' perceptions of cardiovascular risk and the outcomes of preventive therapy in cardiovascular disease". Ann. Intern. Med. 124 (4): 414–21. doi:10.7326/0003-4819-124-4-199602150-00005. PMID 8554250. S2CID 25470460.
- ↑ Laupacis, Andreas (1997). "Clinical prediction rules: a review and suggested modifications of methodological standards". Journal of the American Medical Association. 297: 488–494. doi:10.1001/jama.1997.03540300056034.
- ↑ Bouwmeester W, Zuithoff NP, Mallett S, Geerlings MI, Vergouwe Y, Steyerberg EW, et al. (2012). "Reporting and methods in clinical prediction research: a systematic review". PLOS Med. 9 (5): e1001221. doi: 10.1371/journal.pmed.1001221 . PMC 3358324 . PMID 22629234.
- ↑ Collins GS, Mallett S, Omar O, Yu LM (2011). "Developing risk prediction models for type 2 diabetes: a systematic review of methodology and reporting". BMC Med. 9: 103. doi: 10.1186/1741-7015-9-103 . PMC 3180398 . PMID 21902820.
- ↑ Collins GS, Reitsma HB, Altman DG, Moons KGM. Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): The TRIPOD Statement. Ann Intern Med. 2015;162:55-63
- ↑ Collins GS, Moons KGM, Dhiman P, Riley RD, et al. TRIPOD+AI statement: updated guidance for reporting clinical prediction models that use regression or machine learning methods. BMJ. 2024;385: e078378
- ↑ Reilly BM, Evans AT (2006). "Translating clinical research into clinical practice: impact of using prediction rules to make decisions". Ann. Intern. Med. 144 (3): 201–9. doi:10.7326/0003-4819-144-3-200602070-00009. PMID 16461965. S2CID 32179950.
- ↑ Lee TH, Pearson SD, Johnson PA, et al. (1995). "Failure of information as an intervention to modify clinical management. A time-series trial in patients with acute chest pain". Ann. Intern. Med. 122 (6): 434–7. doi:10.7326/0003-4819-122-6-199503150-00006. PMID 7856992. S2CID 35487553.
- ↑ Poses RM, Cebul RD, Wigton RS (1995). "You can lead a horse to water--improving physicians' knowledge of probabilities may not affect their decisions". Medical Decision Making. 15 (1): 65–75. doi:10.1177/0272989X9501500110. PMID 7898300. S2CID 72016252.
- ↑ Marrie TJ, Lau CY, Wheeler SL, Wong CJ, Vandervoort MK, Feagan BG (2000). "A controlled trial of a critical pathway for treatment of community-acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin". JAMA. 283 (6): 749–55. doi: 10.1001/jama.283.6.749 . PMID 10683053.
- ↑ Yealy DM, Auble TE, Stone RA, et al. (2005). "Effect of increasing the intensity of implementing pneumonia guidelines: a randomized, controlled trial". Ann. Intern. Med. 143 (12): 881–94. doi:10.7326/0003-4819-143-12-200512200-00006. PMID 16365469. S2CID 45414192.