Related Research Articles

Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.

Liver transplantation or hepatic transplantation is the replacement of a diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for end-stage liver disease and acute liver failure, although availability of donor organs is a major limitation. The most common technique is orthotopic transplantation, in which the native liver is removed and replaced by the donor organ in the same anatomic position as the original liver. The surgical procedure is complex, requiring careful harvest of the donor organ and meticulous implantation into the recipient. Liver transplantation is highly regulated, and only performed at designated transplant medical centers by highly trained transplant physicians and supporting medical team. Favorable outcomes require careful screening for eligible recipients, as well as a well-calibrated live or deceased donor match.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.
A Klatskin tumor is a cholangiocarcinoma occurring at the confluence of the right and left hepatic bile ducts. The disease was named after Gerald Klatskin, who in 1965 described 15 cases and found some characteristics for this type of cholangiocarcinoma

Cholangiocarcinoma, also known as bile duct cancer, is a type of cancer that forms in the bile ducts. Symptoms of cholangiocarcinoma may include abdominal pain, yellowish skin, weight loss, generalized itching, and fever. Light colored stool or dark urine may also occur. Other biliary tract cancers include gallbladder cancer and cancer of the ampulla of Vater.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
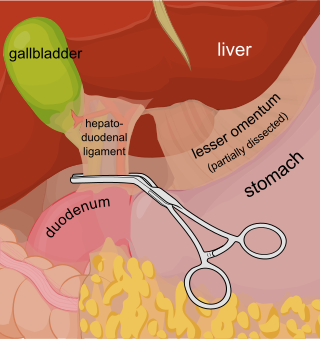
The Pringle manoeuvre is a surgical technique used in some abdominal operations and in liver trauma. The hepatoduodenal ligament is clamped either with a surgical tool called a haemostat, an umbilical tape or by hand. This limits blood inflow through the hepatic artery and the portal vein, controlling bleeding from the liver. It was first published by and named after James Hogarth Pringle in 1908.
Digestive system surgery, or gastrointestinal surgery, can be divided into upper GI surgery and lower GI surgery.

Liver cancer is cancer that starts in the liver. Liver cancer can be primary or secondary. Liver metastasis is more common than that which starts in the liver. Instances of liver cancer are increasing globally.
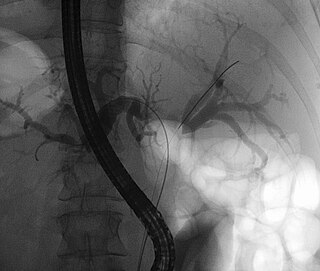
Hepatic arterial infusion (HAI) is a medical procedure that delivers chemotherapy directly to the liver. The procedure, mostly used in combination with systemic chemotherapy, plays a role in the treatment of liver metastases in patients with colorectal cancer (CRC). Although surgical resection remains the standard of care for these liver metastases, majority of patients have lesions that are unresectable.

A liver metastasis is a malignant tumor in the liver that has spread from another organ affected by cancer. The liver is a common site for metastatic disease because of its rich, dual blood supply. Metastatic tumors in the liver are 20 times more common than primary tumors. In 50% of all cases the primary tumor is of the gastrointestinal tract; other common sites include the breast, ovaries, bronchus and kidney. Patients with Colorectal cancer will develop liver metastases during the disease
In oncology, metastasectomy is the surgical removal of metastases, which are secondary cancerous growths that have spread from cancer originating in another organ in the body.
Surgical Outcomes Analysis & Research, SOAR, is a research laboratory of the Department of Surgery at Boston University School of Medicine and Boston Medical Center with expertise in outcomes research. SOAR investigates surgical diseases and perioperative outcomes. The group focuses on pancreatic cancer, other gastrointestinal and hepatobiliary malignancies, vascular disease, and transplant surgery. SOAR's goal is to examine quality, delivery, and financing of care in order to have an immediate impact on patient care and system improvements. The group members utilize national health services and administrative databases, as well as institutional databases, to investigate and to address factors contributing to disease outcomes and healthcare disparities.

Dr. David Geller is the Richard L. Simmons Professor of Surgery at the University of Pittsburgh School of Medicine, and co-director of the UPMC Liver Cancer Center. As a hepatobiliary Surgical Oncologist, his clinical interests center on the evaluation and management of patients with liver cancer. He has pioneered laparoscopic liver resections, and has performed more than 300 of these cases. Most of these patients are discharged home on the second post-operative day with four to five band-aid-sized incisions. He also specializes in performing laparoscopic radiofrequency ablations of liver tumors. Dr. Geller is a member of many professional and scientific societies including the American Surgical Association, Society of Surgical Oncology, Society of University Surgeons, and the American Society of Transplant Surgeons.

Alexey Nikolaevich Severtsev – a Russian doctor of medicine sciences, professor in the hospital surgery department of the medical faculty in Pirogov Russian National Research Medical University and the chief surgeon of a chain of clinics “MEDSI”.
Radiation lobectomy is a form of radiation therapy used in interventional radiology to treat liver cancer. It is performed in patients that would be surgical candidates for resection, but cannot undergo surgery due to insufficient remaining liver tissue. It consists of injecting small radioactive beads loaded with yttrium-90 into the hepatic artery feeding the hepatic lobe in which the tumor is located. This is done with the intent of inducing growth in the contralateral hepatic lobe, not dissimilarly from portal vein embolization (PVE).
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, embolizing agents can be delivered through the tumor’s feeding artery in order to completely occlude the tumor’s blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma (HCC) and/or other hyper-vascular tumors is based on the fact that a normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.

Nuru Bayramov is a surgeon, a professor and head of first department of surgical diseases in Azerbaijan Medical University.

Choledochoduodenostomy (CDD) is a surgical procedure to create an anastomosis, a surgical connection, between the common bile duct (CBD) and an alternative portion of the duodenum. In healthy individuals, the CBD meets the pancreatic duct at the ampulla of Vater, which drains via the major duodenal papilla to the second part of duodenum. In cases of benign conditions such as narrowing of the distal CBD or recurrent CBD stones, performing a CDD provides the diseased patient with CBD drainage and decompression. A side-to-side anastomosis is usually performed.
References
- ↑ Tsuchiya, Ryoichi (2002). "我が国の肝膵外科学 : 1.本庄一夫記念シンポジウムによせて(<特集>創造と調和" [Surgery of the liver and pancreas in Japan--message to the special symposium commemorating Dr. Ichio Honjo]. Nihon Geka Gakkai Zasshi (in Japanese). 103 (3): 318–21. PMID 11968765.
- ↑ Lortat-Jacob, JL; Robert, HG (1952). "Hépatectomie droite réglée" [Well defined technique for right hepatectomy]. La Presse Médicale (in French). 60 (26): 549–51. PMID 14948909.
- ↑ Chang, SB; Palavecino, M; Wray, CJ; Kishi, Y; Pisters, PW; Vauthey, JN (March 2010). "Modified Makuuchi incision for foregut procedures". Archives of Surgery. 145 (3): 281–4. doi:10.1001/archsurg.2010.7. PMID 20231630.
- ↑ Liddo, Guido; Buc, Emmanuel; Nagarajan, Ganesh; Hidaka, Masaaki; Dokmak, Safi; Belghiti, Jacques (2009). "The liver hanging manoeuvre". HPB. 11 (4): 296–305. doi:10.1111/j.1477-2574.2009.00068.x. PMC 2727082 . PMID 19718356.
- ↑ Knipe, Henry; Jones, Jeremy. "Couinaud classification". UBM Medica Network. Retrieved 2 December 2014.
- ↑ International Hepato-Pancreatico-Biliary Association (IHPBA) Terminology for Liver Resections
- ↑ Jarnagin, WR; Gonen, M; Fong, Y; DeMatteo, RP; Ben-Porat, L; Little, S; Corvera, C; Weber, S; Blumgart, LH (October 2002). "Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade". Annals of Surgery. 236 (4): 397–406, discussion 406-7. doi:10.1097/01.SLA.0000029003.66466.B3 (inactive 31 January 2024). PMC 1422593 . PMID 12368667.
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link)