Related Research Articles

Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

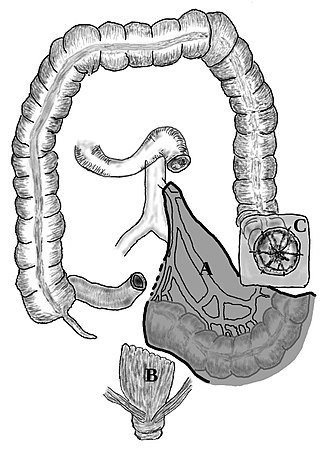
A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.

Diverticulitis, also called colonic diverticulitis, is a gastrointestinal disease characterized by inflammation of abnormal pouches—diverticula—that can develop in the wall of the large intestine. Symptoms typically include lower-abdominal pain of sudden onset, but the onset may also occur over a few days. There may also be nausea; and diarrhea or constipation. Fever or blood in the stool suggests a complication. Repeated attacks may occur.

Colorectal surgery is a field in medicine dealing with disorders of the rectum, anus, and colon. The field is also known as proctology, but this term is now used infrequently within medicine and is most often employed to identify practices relating to the anus and rectum in particular. The word proctology is derived from the Greek words πρωκτός proktos, meaning "anus" or "hindparts", and -λογία -logia, meaning "science" or "study".

A colostomy is an opening (stoma) in the large intestine (colon), or the surgical procedure that creates one. The opening is formed by drawing the healthy end of the colon through an incision in the anterior abdominal wall and suturing it into place. This opening, often in conjunction with an attached ostomy system, provides an alternative channel for feces to leave the body. Thus if the natural anus is unavailable for that function, an artificial anus takes over. It may be reversible or irreversible, depending on the circumstances.
Colectomy is bowel resection of the large bowel (colon). It consists of the surgical removal of any extent of the colon, usually segmental resection. In extreme cases where the entire large intestine is removed, it is called total colectomy, and proctocolectomy denotes that the rectum is included.

Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

Pelvic exenteration is a radical surgical treatment that removes all organs from a person's pelvic cavity. It is used to treat certain advanced or recurrent cancers. The urinary bladder, urethra, rectum, and anus are removed. In women, the vagina, cervix, uterus, Fallopian tubes, ovaries and, in some cases, the vulva are removed. In men, the prostate is removed. The procedure leaves the person with a permanent colostomy and urinary diversion.
A proctosigmoidectomy, Hartmann's operation or Hartmann's procedure is the surgical resection of the rectosigmoid colon with closure of the anorectal stump and formation of an end colostomy. It was used to treat colon cancer or inflammation. Currently, its use is limited to emergency surgery when immediate anastomosis is not possible, or more rarely it is used palliatively in patients with colorectal tumours.
Total mesorectal excision (TME) is a standard surgical technique for treatment of rectal cancer, first described in 1982 by Professor Bill Heald at the UK's Basingstoke District Hospital. It is a precise dissection of the mesorectal envelope comprising rectum containing the tumour together with all the surrounding fatty tissue and the sheet of tissue that contains lymph nodes and blood vessels. Dissection is along the avascular alveolar plane between the presacral and mesorectal fascia, described as holy plane. Dissection along this plane facilitates a straightforward dissection and preserves the sacral vessels and hypogastric nerves and is a sphincter-sparing resection and decreases permanent stoma rates. It is possible to rejoin the two ends of the colon; however, most patients require a temporary ileostomy pouch to bypass the colon, allowing it to heal with less risk of infection, perforation or leakage.

Defecography is a type of medical radiological imaging in which the mechanics of a patient's defecation are visualized in real time using a fluoroscope. The anatomy and function of the anorectum and pelvic floor can be dynamically studied at various stages during defecation.
A lower anterior resection, formally known as anterior resection of the rectum and colon and anterior excision of the rectum or simply anterior resection, is a common surgery for rectal cancer and occasionally is performed to remove a diseased or ruptured portion of the intestine in cases of diverticulitis. It is commonly abbreviated as LAR.
William Ernest Miles was an English surgeon known for the Miles' operation: an abdomino-perineal excision for rectal cancer.
Rectal discharge is intermittent or continuous expression of liquid from the anus. Normal rectal mucus is needed for proper excretion of waste. Otherwise, this is closely related to types of fecal incontinence but the term rectal discharge does not necessarily imply degrees of incontinence. Types of fecal incontinence that produce a liquid leakage could be thought of as a type of rectal discharge.
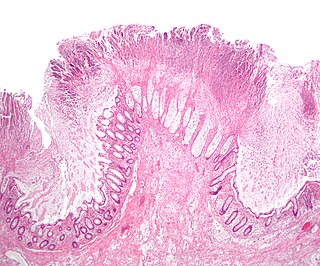
Solitary rectal ulcer syndrome or SRUS is a chronic, benign disorder of the rectal mucosa. It commonly occurs with varying degrees of rectal prolapse. The condition is thought to be caused by different factors, such as long term constipation, straining during defecation, and dyssynergic defecation. Treatment is by normalization of bowel habits, biofeedback, and other conservative measures. In more severe cases various surgical procedures may be indicated. The condition is relatively rare, affecting approximately 1 in 100,000 people per year. It affects mainly adults aged 30–50. Females are affected slightly more often than males. The disorder can be confused clinically with rectal cancer or other conditions such as inflammatory bowel disease, even when a biopsy is done.
Obstructed defecation syndrome is a major cause of functional constipation, of which it is considered a subtype. It is characterized by difficult and/or incomplete emptying of the rectum with or without an actual reduction in the number of bowel movements per week. Normal definitions of functional constipation include infrequent bowel movements and hard stools. In contrast, ODS may occur with frequent bowel movements and even with soft stools, and the colonic transit time may be normal, but delayed in the rectum and sigmoid colon.
Nigro protocol is the preoperative use of chemotherapy with 5-fluorouracil and mitomycin and medical radiation for squamous cell carcinomas of the anal canal. Success of the preoperative regimen changed the paradigm of anal cancer treatment from surgical to non-surgical and was the advent of definitive chemoradiation being accepted as a standard-of-care for anal squamous cell carcinomas. Larger doses of radiation are used in modern chemoradiotherapy protocols versus the original Nigro protocol radiotherapy dose.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.
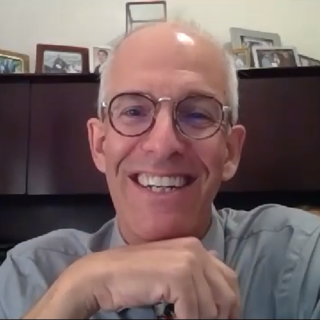
Steven D. Wexner is an American surgeon and physician. He is Director of the Ellen Leifer Shulman and Steven Shulman Digestive Disease Center at Cleveland Clinic Florida. Wexner has received numerous regional, national, and international research awards. Through his multiple academic appointments, Wexner personally trains 15-20 surgeons each year, and he educates thousands more around the world through conferences and lectures. He is a resource for his colleagues from around the world for referral of patients with challenging or complex problems. In 2020, he was elected vice-chair of the Board of Regents of the American College of Surgeons for a one-year term. Since 1990. he has served as Symposium Director of the Cleveland Clinic Annual International Colorectal Disease Symposium. The Symposium was held in Fort Lauderdale or Boca Raton every year from 1990 to 2019. Since 2020, the Symposium has expanded to include host locations outside of the US with interruptions during the pandemic years of 2021–2022.
Low anterior resection syndrome is a complication of lower anterior resection, a type of surgery performed to remove the rectum, typically for rectal cancer. It is characterized by changes to bowel function that affect quality of life, and includes symptoms such as fecal incontinence, incomplete defecation or the sensation of incomplete defecation, changes in stool frequency or consistency, unpredictable bowel function, and painful defecation (dyschezia). Treatment options include symptom management, such as use of enemas, or surgical management, such as creation of a colostomy.
References
- ↑ American Cancer Society. Detailed Guide: Colon and Rectum Cancer. cancer.org. URL: http://www.cancer.org/docroot/CRI/content/CRI_2_4_4x_Surgery_10.asp?sitearea= Archived May 7, 2008, at the Wayback Machine . Accessed on: February 5, 2008.
- ↑ Schrag D, Panageas KS, Riedel E, et al. (November 2002). "Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection". Ann. Surg. 236 (5): 583–92. doi:10.1097/00000658-200211000-00008. PMC 1422616 . PMID 12409664.
- ↑ Marusch F, Koch A, Schmidt U, Pross M, Gastinger I, Lippert H (October 2001). "Hospital caseload and the results achieved in patients with rectal cancer". Br J Surg. 88 (10): 1397–402. doi: 10.1046/j.0007-1323.2001.01873.x . PMID 11578299. S2CID 3095483.
- ↑ Martling A, Holm T, Cedermark B (2005). "[Skills by training. Education and case volume are strong prognostic factors in rectal cancer surgery]". Läkartidningen (in Swedish). 102 (6): 374–6. PMID 15754678.
- ↑ Simorov A, Reynoso JF, Dolghi Thompson JS, Oleynikov D (2011). "Comparison of perioperative outcomes in patients undergoing laparoscopic versus open abdominoperineal resection". Am J Surg. 202 (6): 666–70. doi:10.1016/j.amjsurg.2011.06.029. PMID 21983001.
- ↑ McLeod RS (2001). "Comparison of quality of life in patients undergoing abdominoperineal extirpation or anterior resection for rectal cancer". Ann. Surg. 233 (2): 157–8. doi:10.1097/00000658-200102000-00002. PMC 1421195 . PMID 11176119.
- ↑ Grumann MM, Noack EM, Hoffmann IA, Schlag PM (2001). "Comparison of quality of life in patients undergoing abdominoperineal extirpation or anterior resection for rectal cancer". Ann. Surg. 233 (2): 149–56. doi:10.1097/00000658-200102000-00001. PMC 1421194 . PMID 11176118.
- 1 2 Ganapathi SK, Subbiah R, Rudramurthy S, Kakkilaya H, Ramakrishnan P, Chinnusamy P (2021). "Laparoscopic anterior resection: Analysis of technique over 1000 cases". Journal of Minimal Access Surgery. 17 (3): 356–362. doi:10.4103/jmas.JMAS_132_20. PMC 8270051 . PMID 33605924.
- ↑ Miles, W. E. (1971). "A Method of Performing Abdomino-Perineal Excision for Carcinoma of the Rectum and of the Terminal Portion of the Pelvic Colon (1908)". CA: A Cancer Journal for Clinicians. 21 (6): 361–364. doi: 10.3322/canjclin.21.6.361 . PMID 5001853. S2CID 73293240.