Related Research Articles
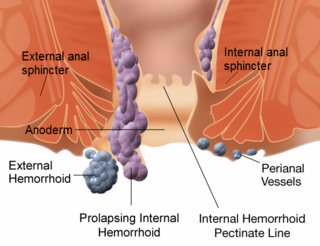
Hemorrhoids, also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term "hemorrhoid" is often used to refer to the disease. The signs and symptoms of hemorrhoids depend on the type present. Internal hemorrhoids often result in painless, bright red rectal bleeding when defecating. External hemorrhoids often result in pain and swelling in the area of the anus. If bleeding occurs, it is usually darker. Symptoms frequently get better after a few days. A skin tag may remain after the healing of an external hemorrhoid.

Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits, and receptive anal sex. An estimated 2.2% of community dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

Coronary artery bypass surgery, also known as coronary artery bypass graftsurgery, and colloquially heart bypass or bypass surgery, is a surgical procedure to restore normal blood flow to an obstructed coronary artery. A normal coronary artery transports blood to the heart muscle itself, not through the main circulatory system.
An anal fissure is a break or tear in the skin of the anal canal. Anal fissures may be noticed by bright red anal bleeding on toilet paper and undergarments, or sometimes in the toilet. If acute they are painful after defecation, but with chronic fissures, pain intensity often reduces. Anal fissures usually extend from the anal opening and are usually located posteriorly in the midline, probably because of the relatively unsupported nature and poor perfusion of the anal wall in that location. Fissure depth may be superficial or sometimes down to the underlying sphincter muscle. Untreated fissures develop a hood-like skin tag which cover the fissure and cause discomfort and pain.

In surgery or medical procedure, a ligature consists of a piece of thread (suture) tied around an anatomical structure, usually a blood vessel or another hollow structure to shut it off.

A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.

Colorectal surgery is a field in medicine dealing with disorders of the rectum, anus, and colon. The field is also known as proctology, but this term is now used infrequently within medicine and is most often employed to identify practices relating to the anus and rectum in particular. The word proctology is derived from the Greek words πρωκτός proktos, meaning "anus" or "hindparts", and -λογία -logia, meaning "science" or "study".

Anal fistula is a chronic abnormal communication between the epithelialised surface of the anal canal and usually the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.

The middle rectal artery is an artery in the pelvis that supplies blood to the rectum.

Diosmin, a flavone glycoside of diosmetin, is manufactured from citrus fruit peels as a phlebotonic non-prescription dietary supplement used to aid treatment of hemorrhoids or chronic venous diseases, mainly of the legs.
Mastopexy is the plastic surgery mammoplasty procedure for raising sagging breasts upon the chest of the woman, by changing and modifying the size, contour, and elevation of the breasts. In a breast-lift surgery to re-establish an aesthetically proportionate bust for the woman, the critical corrective consideration is the tissue viability of the nipple-areola complex (NAC), to ensure the functional sensitivity of the breasts for lactation and breast-feeding.

A surgical anastomosis is a surgical technique used to make a new connection between two body structures that carry fluid, such as blood vessels or bowel. For example, an arterial anastomosis is used in vascular bypass and a colonic anastomosis is used to restore colonic continuity after the resection of colon cancer.

Stapled hemorrhoidopexy is a surgical procedure that involves the cutting and removal of anal hemorrhoidal vascular cushion, whose function is to help to seal stools and create continence. Procedure also removes abnormally enlarged hemorrhoidal tissue, followed by the repositioning of the remaining hemorrhoidal tissue back to its normal anatomic position. Severe cases of hemorrhoidal prolapse will normally require surgery. Newer surgical procedures include stapled transanal rectal resection (STARR) and procedure for prolapse and hemorrhoids (PPH). Both STARR and PPH are contraindicated in persons with either enterocele or anismus.
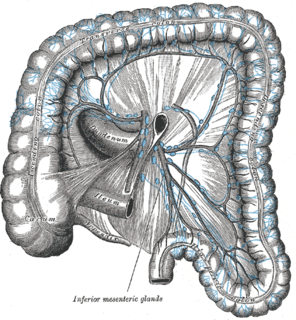
The inferior mesenteric lymph nodes consist of:

The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about 12 centimetres (4.7 in) long, and begins at the rectosigmoid junction at the level of the third sacral vertebra or the sacral promontory depending upon what definition is used. Its diameter is similar to that of the sigmoid colon at its commencement, but it is dilated near its termination, forming the rectal ampulla. It terminates at the level of the anorectal ring or the dentate line, again depending upon which definition is used. In humans, the rectum is followed by the anal canal which is about 4 centimetres (1.6 in) long, before the gastrointestinal tract terminates at the anal verge. The word rectum comes from the Latin rectumintestinum, meaning straight intestine.

In humans, the anus is the external opening of the rectum, located inside the intergluteal cleft and separated from the genitals by the perineum. Two sphincters control the exit of feces from the body during an act of defecation, which is the primary function of the anus. These are the internal anal sphincter and the external anal sphincter, which are circular muscles that normally maintain constriction of the orifice and which relaxes as required by normal physiological functioning. The inner sphincter is involuntary and the outer is voluntary. It is located behind the perineum which is located behind the vagina or scrotum.
Anorectal varices are the dilation of collateral submucosal vessels due to backflow in the veins of the rectum. Typically this occurs due to portal hypertension which shunts venous blood from the portal system through the portosystemic anastomosis present at this site into the systemic venous system. This can also occur in the esophagus, causing esophageal varices, and at the level of the umbilicus, causing caput medusae. Between 44% and 78% of patients with portal hypertension get anorectal varices.

Paolo Antonio Boccasanta is an Italian general surgeon, a professor at the University of Milan and a specialist in general, vascular and thoracic surgery. He took a qualification in Coloproctology in 2000 in Brighton (UK) from the European Board of Surgery.
Transanal irrigation of the rectum and colon is designed to assist the evacuation of feces from the bowel by introducing water into these compartments via the anus.

A. K. M. Fazlul Haque is a Bangladeshi surgeon. He was the founder of the Department of Colorectal Surgery in Bangabandhu Sheikh Mujib Medical University (BSMMU) in Dhaka.
References
- ↑ Morinaga K, Hasuda K, Ikeda T (April 1995). "A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter". Am. J. Gastroenterol. 90 (4): 610–3. PMID 7717320.
- 1 2 "Transanal Hemorrhoidal Dearterialization (THD): Can ligate and lift replace cut and stitch? A new trick for an old problem". Los Angeles Colon and Rectal Surgical Associates. 2012.
- ↑ Dal Monte PP, Tagariello C, Sarago M, et al. (December 2007). "Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease". Tech Coloproctol. 11 (4): 333–8, discussion 338–9. doi:10.1007/s10151-007-0376-4. PMID 18060529. S2CID 9074909.
- ↑ Infantino A, Bellomo R, Dal Monte PP, et al. (August 2010). "Transanal haemorrhoidal artery echodoppler ligation and anopexy (THD) is effective for II and III degree haemorrhoids: a prospective multicentric study". Colorectal Disease. 12 (8): 804–9. doi:10.1111/j.1463-1318.2009.01915.x. PMID 19508513. S2CID 25319116.
- ↑ Sohn N, Aronoff JS, Cohen FS, Weinstein MA (November 2001). "Transanal hemorrhoidal dearterialization is an alternative to operative hemorrhoidectomy". Am. J. Surg. 182 (5): 515–9. doi:10.1016/s0002-9610(01)00759-0. PMID 11754861.
- ↑ Ratto C, Donisi L, Parello A, Litta F, Doglietto GB (May 2010). "Evaluation of Transanal Hemorrhoidal Dearterialization as a Minimally Invasive Therapeutic Approach to Hemorrhoids". Dis. Colon Rectum. 53 (5): 803–11. doi:10.1007/DCR.0b013e3181cdafa7. PMID 20389215. S2CID 27789593.
- ↑ Giordano P, Overton J, Madeddu F, Zaman S, Gravante G (September 2009). "Transanal hemorrhoidal dearterialization: a systematic review". Dis. Colon Rectum. 52 (9): 1665–71. doi:10.1007/DCR.0b013e3181af50f4. PMID 19690499. S2CID 13116518.
- ↑ Loganathan, Arun; Das, Atandrilla; Luck, Andrew; Hewett, Peter (January 2016). "Transanal haemorrhoidal dearterialization for the treatment of grade III and IV haemorrhoids: a 3-year experience". ANZ Journal of Surgery. 86 (1–2): 59–62. doi:10.1111/ans.12816. ISSN 1445-2197. PMID 25142863. S2CID 1425574.