Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver. The digestive system functions to move material through the GI tract via peristalsis, break down that material via digestion, absorb nutrients for use throughout the body, and remove waste from the body via defecation. Physicians who specialize in the medical specialty of gastroenterology are called gastroenterologists or sometimes GI doctors. Some of the most common conditions managed by gastroenterologists include gastroesophageal reflux disease, gastrointestinal bleeding, irritable bowel syndrome, inflammatory bowel disease (IBD) which includes Crohn's disease and ulcerative colitis, peptic ulcer disease, gallbladder and biliary tract disease, hepatitis, pancreatitis, colitis, colon polyps and cancer, nutritional problems, and many more.
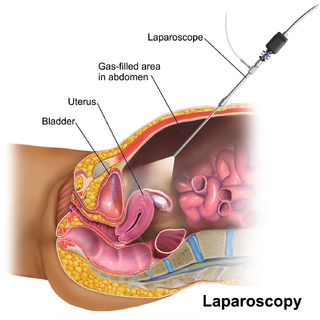
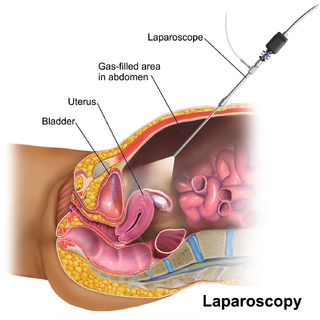
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.
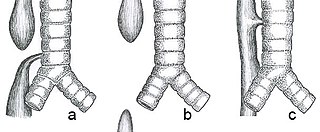
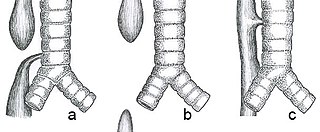
Esophageal atresia is a congenital medical condition that affects the alimentary tract. It causes the esophagus to end in a blind-ended pouch rather than connecting normally to the stomach. It comprises a variety of congenital anatomic defects that are caused by an abnormal embryological development of the esophagus. It is characterized anatomically by a congenital obstruction of the esophagus with interruption of the continuity of the esophageal wall.

Nasogastric intubation is a medical process involving the insertion of a plastic tube through the nose, down the esophagus, and down into the stomach. Orogastric intubation is a similar process involving the insertion of a plastic tube through the mouth. Abraham Louis Levin invented the NG tube. Nasogastric tube is also known as Ryle's tube in Commonwealth countries, after John Alfred Ryle.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

A feeding tube is a medical device used to provide nutrition to people who cannot obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. The state of being fed by a feeding tube is called gavage, enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units. They are classified by the site of insertion and intended use.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.

A Gastrostomy is the creation of an artificial external opening into the stomach for nutritional support or gastric decompression. Typically this would include an incision in the patient's epigastrium as part of a formal operation. When originally devised over a century ago the procedure was completed through open surgery using the Stamm technique. It can be performed through surgical approach, percutaneous approach by interventional radiology, percutaneous endoscopic gastrostomy (PEG) or percutaneous ultrasound gastrostomy (PUG).

Pseudocysts are like cysts, but lack epithelial or endothelial cells. Initial management consists of general supportive care. Symptoms and complications caused by pseudocysts require surgery. Computed tomography (CT) scans are used for initial imaging of cysts, and endoscopic ultrasounds are used in differentiating between cysts and pseudocysts. Endoscopic drainage is a popular and effective method of treating pseudocysts.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.
Gastroparesis, also called delayed gastric emptying, is a medical disorder consisting of weak muscular contractions (peristalsis) of the stomach, resulting in food and liquid remaining in the stomach for a prolonged period of time. Stomach contents thus exit more slowly into the duodenum of the digestive tract. This can result in irregular absorption of nutrients, inadequate nutrition, and poor glycemic control.
A tracheo-esophageal puncture is a surgically created hole between the trachea (windpipe) and the esophagus in a person who has had a total laryngectomy, a surgery where the larynx is removed. The purpose of the puncture is to restore a person’s ability to speak after the vocal cords have been removed. This involves creation of a fistula between trachea and oesophagus, puncturing the short segment of tissue or “common wall” that typically separates these two structures. A voice prosthesis is inserted into this puncture. The prosthesis keeps food out of the trachea but lets air into the esophagus for oesophageal speech.

Stomach diseases include gastritis, gastroparesis, Crohn's disease and various cancers.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.

Jejunostomy is the surgical creation of an opening (stoma) through the skin at the front of the abdomen and the wall of the jejunum. It can be performed either endoscopically, or with open surgery.

A gastric balloon, also known as an intragastric balloon (IGB) or a stomach balloon, is an inflatable medical device that is temporarily placed into the stomach to help reduce weight. It is designed to help provide weight loss when diet and exercise have failed and surgery is not wanted or not recommended for the patient.

Cancer and nausea are associated in about fifty percent of people affected by cancer. This may be as a result of the cancer itself, or as an effect of the treatment such as chemotherapy, radiation therapy, or other medication such as opiates used for pain relief. About 70 to 80% of people undergoing chemotherapy experience nausea or vomiting. Nausea and vomiting may also occur in people not receiving treatment, often as a result of the disease involving the gastrointestinal tract, electrolyte imbalance, or as a result of anxiety. Nausea and vomiting may be experienced as the most unpleasant side effects of cytotoxic drugs and may result in patients delaying or refusing further radiotherapy or chemotherapy.
Buried bumper syndrome (BBS) is a condition that affects feeding tubes placed into the stomach through the abdominal wall. Gastrostomy tubes include an internal bumper, which secures the inner portion of the tube inside the stomach, and external bumper, which secures the outer portion of the tube and opposes the abdomen. Buried bumper syndrome occurs when the internal bumper of a gastrostomy tube erodes into the wall of the stomach. The internal bumper may become entirely buried within the fistulous tract. The main causative factor is excessive tightening of the external bumper, leading to increased pressure of the internal bumper on the wall of the stomach. Additional risk factors include: obesity, weight gain, malnutrition, corticosteroid therapy, and poor wound healing.