Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.

The gastrointestinal tract is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organs of the digestive system, in humans and other animals, including the esophagus, stomach, and intestines. Food taken in through the mouth is digested to extract nutrients and absorb energy, and the waste expelled at the anus as faeces. Gastrointestinal is an adjective meaning of or pertaining to the stomach and intestines.

The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In mammals it may be the principal site for iron absorption. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.

A lower gastrointestinal series is a medical procedure used to examine and diagnose problems with the human colon of the large intestine. Radiographs are taken while barium sulfate, a radiocontrast agent, fills the colon via an enema through the rectum.

Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal tract. GISTs arise in the smooth muscle pacemaker interstitial cell of Cajal, or similar cells. They are defined as tumors whose behavior is driven by mutations in the KIT gene (85%), PDGFRA gene (10%), or BRAF kinase (rare). 95% of GISTs stain positively for KIT (CD117). Most (66%) occur in the stomach and gastric GISTs have a lower malignant potential than tumors found elsewhere in the GI tract.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.
Radiocontrast agents are substances used to enhance the visibility of internal structures in X-ray-based imaging techniques such as computed tomography, projectional radiography, and fluoroscopy. Radiocontrast agents are typically iodine, or more rarely barium sulfate. The contrast agents absorb external X-rays, resulting in decreased exposure on the X-ray detector. This is different from radiopharmaceuticals used in nuclear medicine which emit radiation.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.
Dumping syndrome occurs when food, especially sugar, moves too quickly from the stomach to the duodenum—the first part of the small intestine—in the upper gastrointestinal (GI) tract. This condition is also called rapid gastric emptying. It is mostly associated with conditions following gastric or esophageal surgery, though it can also arise secondary to diabetes or to the use of certain medications; it is caused by an absent or insufficiently functioning pyloric sphincter, the valve between the stomach and the duodenum.

Virtual colonoscopy is the use of CT scanning or magnetic resonance imaging (MRI) to produce two- and three-dimensional images of the colon, from the lowest part, the rectum, to the lower end of the small intestine, and to display the images on an electronic display device. The procedure is used to screen for colon cancer and polyps, and may detect diverticulosis. A virtual colonoscopy can provide 3D reconstructed endoluminal views of the bowel. VC provides a secondary benefit of revealing diseases or abnormalities outside the colon.

Gastrointestinal perforation, also known as gastrointestinal rupture, is a hole in the wall of the gastrointestinal tract. The gastrointestinal tract is composed of hollow digestive organs leading from the mouth to the anus. Symptoms of gastrointestinal perforation commonly include severe abdominal pain, nausea, and vomiting. Complications include a painful inflammation of the inner lining of the abdominal wall and sepsis.

Diatrizoate, also known as amidotrizoate, Gastrografin, is a contrast agent used during X-ray imaging. This includes visualizing veins, the urinary system, spleen, and joints, as well as computer tomography. It is given by mouth, injection into a vein, injection into the bladder, through a nasogastric tube, or rectally.

Intestinal pseudo-obstruction (IPO) is a clinical syndrome caused by severe impairment in the ability of the intestines to push food through. It is characterized by the signs and symptoms of intestinal obstruction without any lesion in the intestinal lumen. Clinical features mimic those seen with mechanical intestinal obstructions and can include abdominal pain, nausea, abdominal distension, vomiting, dysphagia and constipation depending upon the part of the gastrointestinal tract involved.

Barium sulfate suspension, often simply called barium, is a contrast agent used during X-rays. Specifically it is used to improve visualization of the gastrointestinal tract on plain X-ray or computed tomography. It is taken by mouth or used rectally.

Capsule endoscopy is a medical procedure used to record internal images of the gastrointestinal tract for use in disease diagnosis. Newer developments are also able to take biopsies and release medication at specific locations of the entire gastrointestinal tract. Unlike the more widely used endoscope, capsule endoscopy provides the ability to see the middle portion of the small intestine. It can be applied to the detection of various gastrointestinal cancers, digestive diseases, ulcers, unexplained bleedings, and general abdominal pains. After a patient swallows the capsule, it passes along the gastrointestinal tract, taking a number of images per second which are transmitted wirelessly to an array of receivers connected to a portable recording device carried by the patient. General advantages of capsule endoscopy over standard endoscopy include the minimally invasive procedure setup, ability to visualize more of the gastrointestinal tract, and lower cost of the procedure.

An abdominal x-ray is an x-ray of the abdomen. It is sometimes abbreviated to AXR, or KUB.

Gastroparesis, also called delayed gastric emptying is a medical disorder consisting of weak muscular contractions (peristalsis) of the stomach, resulting in food and liquid remaining in the stomach for a prolonged period of time. Stomach contents thus exit more slowly into the duodenum of the digestive tract. This can result in irregular absorption of nutrients, inadequate nutrition, and poor glycemic control. The opposite of this, where stomach contents exit quickly into the duodenum is called dumping syndrome.

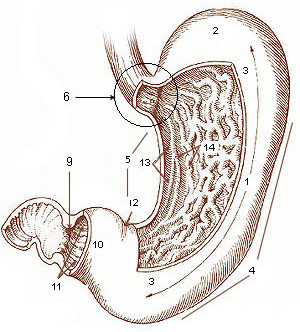
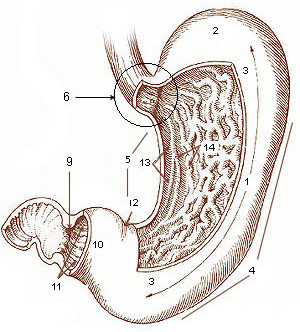
The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion. Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.
Magnetic resonance enterography is a magnetic resonance imaging technique used to evaluate bowel wall features of both upper and lower gastro-intestinal tract, although it is usually used for small bowel evaluation. It is a less invasive technique with the advantages of no ionizing radiation exposure, multiplanarity and high contrast resolution for soft tissue.
Computed tomography enterography is a medical imaging technique which uses computed tomography scanner and contrast media to examine the small bowel. It was first introduced by Raptopoulos et al. in 1997. CT Enterography can be used to assess a variety of problems involving the small bowel, however it is mainly used to diagnose and assess severity of Crohn's disease.