Related Research Articles

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of Achalasia exist, but this is neither fully understood, nor agreed upon.
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid into the esophagus. It is the major symptom of gastroesophageal reflux disease (GERD).
An esophageal motility disorder (EMD) is any medical disorder causing difficulty in swallowing, regurgitation of food and a spasm-type pain which can be brought on by an allergic reaction to certain foods. The most prominent one is dysphagia.

Gastroesophageal reflux disease (GERD), is a chronic condition in which stomach contents rise up into the esophagus, resulting in symptoms and/or complications. Symptoms include the taste of acid in the back of the mouth, heartburn, bad breath, chest pain, regurgitation, breathing problems, and wearing away of the teeth. Complications include esophagitis, esophageal stricture, and Barrett's esophagus.
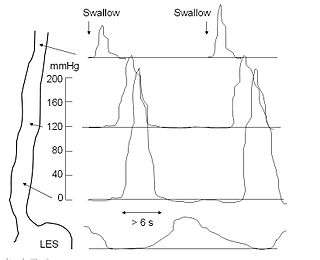
An esophageal motility study (EMS) or esophageal manometry is a test to assess motor function of the upper esophageal sphincter (UES), esophageal body and lower esophageal sphincter (LES).

Esophagogastroduodenoscopy, also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
Esophageal dilatation is a therapeutic endoscopic procedure that enlarges the lumen of the esophagus.
Esophageal spasm is a disorder of motility of the esophagus.

Nutcracker esophagus, or hypertensive peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, to both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.

High-resolution manometry (HRM) is a gastrointestinal motility diagnostic system that measures intraluminal pressure activity in the gastrointestinal tract using a series of closely spaced pressure sensors. For a manometry system to be classified as "high-resolution" as opposed to "conventional", the pressure sensors need to be spaced at most 1 cm apart. Two dominant pressure transduction technologies are used: solid state pressure sensors and water perfused pressure sensors. Each pressure transduction technology has its own inherent advantages and disadvantages. HRM systems also require advanced computer hardware and software to store and analyze the manometry data.

An esophageal food bolus obstruction is a medical emergency caused by the obstruction of the esophagus by an ingested foreign body.

Given Imaging is an Israeli medical technology company that manufactures and markets diagnostic products for the visualization and detection of disorders of the gastrointestinal tract. Until March 2014, it was dual-listed on both the NASDAQ and the Tel Aviv Stock Exchange, where it was a component of the TA-100 Index and the TA BlueTech Index. In March 2014 it was acquired by Covidien and became a private company. In 2015 Covidien was purchased by Medtronic.

Esophageal pH monitoring is the current gold standard for diagnosis of gastroesophageal reflux disease (GERD). It provides direct physiologic measurement of acid in the esophagus and is the most objective method to document reflux disease, assess the severity of the disease and monitor the response of the disease to medical or surgical treatment. It can also be used in diagnosing laryngopharyngeal reflux.
Anorectal manometry(ARM) is a medical test used to measure pressures in the anus and rectum and to assess their function. The test is performed by inserting a catheter, that contains a probe embedded with pressure sensors, through the anus and into the rectum. Patients may be asked to perform certain maneuvers, such as coughing or attempting to defecate, to assess for pressure changes. Anorectal manometry is a safe and low risk procedure.

Esophageal intramucosal pseudodiverticulosis (EIPD) is a rare condition wherein the wall of the esophagus develops numerous small outpouchings (pseudodiverticulae). Individuals with the condition typically develop difficulty swallowing. The outpouchings represent the ducts of submucosal glands of the esophagus. It typically affects individuals in their sixth and seventh decades of life. While it is associated with certain chronic conditions, particularly alcoholism, diabetes and gastroesophageal reflux disease, the cause of the condition is unknown. Treatment involves medications to treat concomitant conditions such as reflux and esophageal spasm, and dilation of strictures in the esophagus.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.

Satish Sanku Chander Rao is the J.Harold Harrison Distinguished University Chair in Gastroenterology at the Medical College of Georgia, Augusta University. He served as the former President of the American Neurogastroenterology and Motility Society and as Chair of the American Gastroenterological Association (AGA) Institute Council, Neurogastroenterology/Motility Section.
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractor symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Savarino, E; di Pietro, M; Bredenoord, AJ; Carlson, DA; Clarke, JO; Khan, A; Vela, MF; Yadlapati, R; Pohl, D; Pandolfino, JE; Roman, S; Gyawali, CP (November 2020). "Use of the Functional Lumen Imaging Probe in Clinical Esophagology". The American Journal of Gastroenterology. 115 (11): 1786–1796. doi: 10.14309/ajg.0000000000000773 . PMID 33156096.
- ↑ Yadlapati, R; Kahrilas, PJ; Fox, MR; Bredenoord, AJ; Prakash Gyawali, C; Roman, S; Babaei, A; Mittal, RK; Rommel, N; Savarino, E; Sifrim, D; Smout, A; Vaezi, MF; Zerbib, F; Akiyama, J; Bhatia, S; Bor, S; Carlson, DA; Chen, JW; Cisternas, D; Cock, C; Coss-Adame, E; de Bortoli, N; Defilippi, C; Fass, R; Ghoshal, UC; Gonlachanvit, S; Hani, A; Hebbard, GS; Wook Jung, K; Katz, P; Katzka, DA; Khan, A; Kohn, GP; Lazarescu, A; Lengliner, J; Mittal, SK; Omari, T; Park, MI; Penagini, R; Pohl, D; Richter, JE; Serra, J; Sweis, R; Tack, J; Tatum, RP; Tutuian, R; Vela, MF; Wong, RK; Wu, JC; Xiao, Y; Pandolfino, JE (January 2021). "Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©" (PDF). Neurogastroenterology and Motility. 33 (1): e14058. doi:10.1111/nmo.14058. PMC 8034247 . PMID 33373111.CS1 maint: PMC embargo expired (link)
- ↑ Hirano, I; Pandolfino, JE; Boeckxstaens, GE (March 2017). "Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute". Clinical Gastroenterology and Hepatology. 15 (3): 325–334. doi:10.1016/j.cgh.2016.10.022. PMC 5757507 . PMID 28212976.
- ↑ Massey, BT (November 2020). "Clinical Functional Lumen Imaging Probe Testing in Esophageal Disorders: A Need for Better Quality Evidence". The American Journal of Gastroenterology. 115 (11): 1799–1801. doi:10.14309/ajg.0000000000000974. PMID 33156098.
- ↑ Massey, BT (10 July 2020). "Flip Technology for Assessing Esophageal Structural and Motor Disorders: a Skeptic's View". Current Gastroenterology Reports. 22 (9): 44. doi:10.1007/s11894-020-00782-2. PMID 32651682. S2CID 220462184.
- ↑ Gregersen, H; Lo, KM (30 April 2018). "What Is the Future of Impedance Planimetry in Gastroenterology?". Journal of Neurogastroenterology and Motility. 24 (2): 166–181. doi: 10.5056/jnm18013 . PMC 5885717 . PMID 29605974.
- 1 2 DeVault, KR (December 2019). "Functional luminal imaging probe: an evolving technology for the diagnosis of esophageal motility disorders". Gastrointestinal Endoscopy. 90 (6): 924–925. doi: 10.1016/j.gie.2019.08.025 . PMID 31759418.