Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Abdominal pain, also known as a stomach ache, Is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

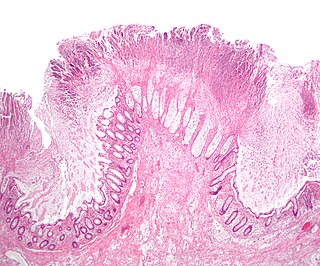
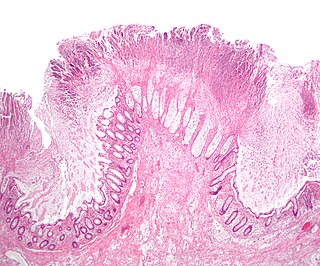
Diverticulitis, also called colonic diverticulitis, is a gastrointestinal disease characterized by inflammation of abnormal pouches—diverticula—that can develop in the wall of the large intestine. Symptoms typically include lower-abdominal pain of sudden onset, but the onset may also occur over a few days. There may also be nausea; and diarrhea or constipation. Fever or blood in the stool suggests a complication. Repeated attacks may occur.

A Meckel's diverticulum, a true congenital diverticulum, is a slight bulge in the small intestine present at birth and a vestigial remnant of the vitelline duct. It is the most common malformation of the gastrointestinal tract and is present in approximately 2% of the population, with males more frequently experiencing symptoms.

Short bowel syndrome is a rare malabsorption disorder caused by a lack of functional small intestine. The primary symptom is diarrhea, which can result in dehydration, malnutrition, and weight loss. Other symptoms may include bloating, heartburn, feeling tired, lactose intolerance, and foul-smelling stool. Complications can include anemia and kidney stones.
Colic in horses is defined as abdominal pain, but it is a clinical symptom rather than a diagnosis. The term colic can encompass all forms of gastrointestinal conditions which cause pain as well as other causes of abdominal pain not involving the gastrointestinal tract. What makes it tricky is that different causes can manifest with similar signs of distress in the animal. Recognizing and understanding these signs is pivotal, as timely action can spell the difference between a brief moment of discomfort and a life-threatening situation. The most common forms of colic are gastrointestinal in nature and are most often related to colonic disturbance. There are a variety of different causes of colic, some of which can prove fatal without surgical intervention. Colic surgery is usually an expensive procedure as it is major abdominal surgery, often with intensive aftercare. Among domesticated horses, colic is the leading cause of premature death. The incidence of colic in the general horse population has been estimated between 4 and 10 percent over the course of the average lifespan. Clinical signs of colic generally require treatment by a veterinarian. The conditions that cause colic can become life-threatening in a short period of time.

Intussusception is a medical condition in which a part of the intestine folds into the section immediately ahead of it. It typically involves the small bowel and less commonly the large bowel. Symptoms include abdominal pain which may come and go, vomiting, abdominal bloating, and bloody stool. It often results in a small bowel obstruction. Other complications may include peritonitis or bowel perforation.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.
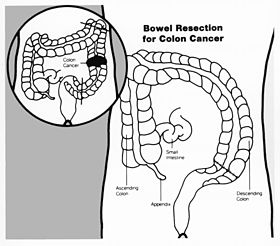
Colectomy is bowel resection of the large bowel (colon). It consists of the surgical removal of any extent of the colon, usually segmental resection. In extreme cases where the entire large intestine is removed, it is called total colectomy, and proctocolectomy denotes that the rectum is included.

Gastrointestinal perforation, also known as ruptured bowel, is a hole in the wall of part of the gastrointestinal tract. The gastrointestinal tract includes the esophagus, stomach, small intestine, and large intestine. Symptoms include severe abdominal pain and tenderness. The pain is typically sudden when the hole is in the stomach or duodenum, whereas the pain may occur more gradually when the hole in the large intestine. The pain is usually constant in nature. Sepsis, with an increased heart rate, increased breathing rate, fever, and confusion may occur.
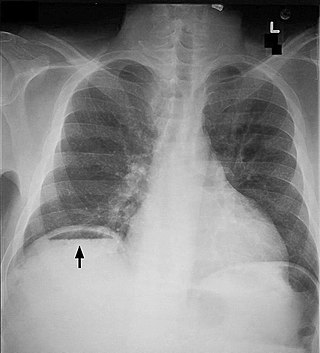
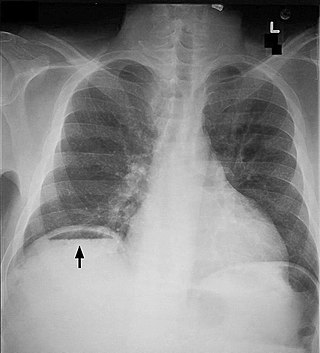
Pneumoperitoneum is pneumatosis in the peritoneal cavity, a potential space within the abdominal cavity. The most common cause is a perforated abdominal organ, generally from a perforated peptic ulcer, although any part of the bowel may perforate from a benign ulcer, tumor or abdominal trauma. A perforated appendix seldom causes a pneumoperitoneum.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.
An acute abdomen refers to a sudden, severe abdominal pain. It is in many cases a medical emergency, requiring urgent and specific diagnosis. Several causes need immediate surgical treatment.

A surgical anastomosis is a surgical technique used to make a new connection between two body structures that carry fluid, such as blood vessels or bowel. For example, an arterial anastomosis is used in vascular bypass and a colonic anastomosis is used to restore colonic continuity after the resection of colon cancer.

Bowel infarction or gangrenous bowel represents an irreversible injury to the intestine resulting from insufficient blood flow. It is considered a medical emergency because it can quickly result in life-threatening infection and death. Any cause of bowel ischemia, the earlier reversible form of injury, may ultimately lead to infarction if uncorrected. The causes of bowel ischemia or infarction include primary vascular causes and other causes of bowel obstruction.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.
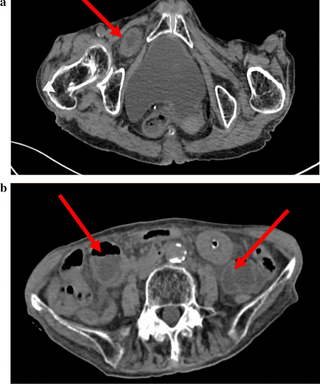
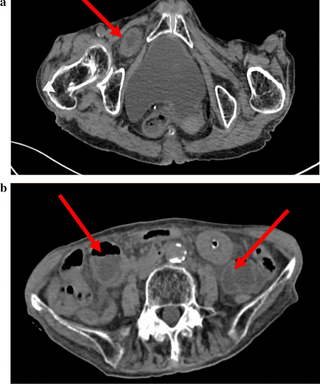
An obturator hernia is a rare type of hernia, encompassing 0.07-1% of all hernias, of the pelvic floor in which pelvic or abdominal contents protrudes through the obturator foramen. The obturator foramen is formed by a branch of the ischial as well as the pubic bone. The canal is typically 2-3 centimeters long and 1 centimeters wide, creating a space for pouches of pre-peritoneal fat.

Jejunostomy is the surgical creation of an opening (stoma) through the skin at the front of the abdomen and the wall of the jejunum. It can be performed either endoscopically, or with open surgery.

Internal hernias occur when there is protrusion of an internal organ into a retroperitoneal fossa or a foramen in the abdominal cavity. If a loop of bowel passes through the mesenteric defect, that loop is at risk for incarceration, strangulation, or for becoming the lead point of a small bowel obstruction. Internal hernias can also trap adipose tissue (fat) and nerves. Unlike more common forms of hernias, the trapped tissue protrudes inward, rather than outward.

Sigmoid colon volvulus, also known as sigmoid volvulus, is volvulus affecting the sigmoid colon. It is a common cause of bowel obstruction and constipation. It is common in Asia, India and especially South India because of the high fibre diet. It is a very common cause of large bowel obstruction in Peru and Bolivia due to high altitude.