Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.
A hernia is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. The term is also used for the normal development of the intestinal tract, referring to the retraction of the intestine from the extra-embryonal navel coelom into the abdomen in the healthy embryo at about 7½ weeks.
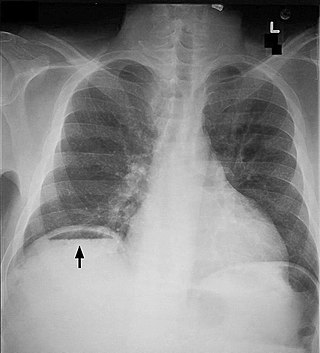
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.
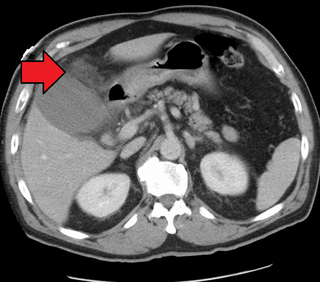
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks precede acute cholecystitis. The pain lasts longer in cholecystitis than in a typical gallbladder attack. Without appropriate treatment, recurrent episodes of cholecystitis are common. Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.
Colic in horses is defined as abdominal pain, but it is a clinical symptom rather than a diagnosis. The term colic can encompass all forms of gastrointestinal conditions which cause pain as well as other causes of abdominal pain not involving the gastrointestinal tract. What makes it tricky is that different causes can manifest with similar signs of distress in the animal. Recognizing and understanding these signs is pivotal, as timely action can spell the difference between a brief moment of discomfort and a life-threatening situation. The most common forms of colic are gastrointestinal in nature and are most often related to colonic disturbance. There are a variety of different causes of colic, some of which can prove fatal without surgical intervention. Colic surgery is usually an expensive procedure as it is major abdominal surgery, often with intensive aftercare. Among domesticated horses, colic is the leading cause of premature death. The incidence of colic in the general horse population has been estimated between 4 and 10 percent over the course of the average lifespan. Clinical signs of colic generally require treatment by a veterinarian. The conditions that cause colic can become life-threatening in a short period of time.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:

An umbilical hernia is a health condition where the abdominal wall behind the navel is damaged. It may cause the navel to bulge outwards—the bulge consisting of abdominal fat from the greater omentum or occasionally parts of the small intestine. The bulge can often be pressed back through the hole in the abdominal wall, and may "pop out" when coughing or otherwise acting to increase intra-abdominal pressure. Treatment is surgical, and surgery may be performed for cosmetic as well as health-related reasons.
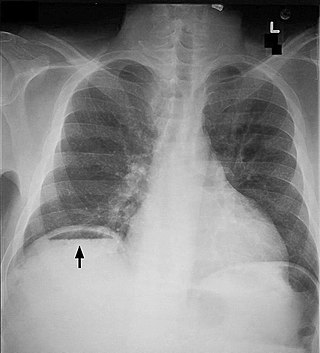
Pneumoperitoneum is pneumatosis in the peritoneal cavity, a potential space within the abdominal cavity. The most common cause is a perforated abdominal organ, generally from a perforated peptic ulcer, although any part of the bowel may perforate from a benign ulcer, tumor or abdominal trauma. A perforated appendix seldom causes a pneumoperitoneum.
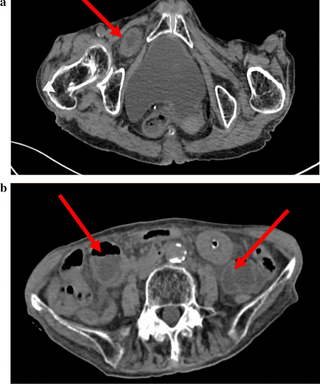
Femoral hernias occur just below the inguinal ligament, when abdominal contents pass through a naturally occurring weakness in the abdominal wall called the femoral canal. Femoral hernias are a relatively uncommon type, accounting for only 3% of all hernias. While femoral hernias can occur in both males and females, almost all develop in women due to the increased width of the female pelvis. Femoral hernias are more common in adults than in children. Those that do occur in children are more likely to be associated with a connective tissue disorder or with conditions that increase intra-abdominal pressure. Seventy percent of pediatric cases of femoral hernias occur in infants under the age of one.
An acute abdomen refers to a sudden, severe abdominal pain. It is in many cases a medical emergency, requiring urgent and specific diagnosis. Several causes need immediate surgical treatment.

A bowel resection or enterectomy is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel ischemia, necrosis, or obstruction due to scar tissue, volvulus, and hernias. Some patients require ileostomy or colostomy after this procedure as alternative means of excretion. Complications of the procedure may include anastomotic leak or dehiscence, hernias, or adhesions causing partial or complete bowel obstruction. Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.

Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected.

Bowel infarction or gangrenous bowel represents an irreversible injury to the intestine resulting from insufficient blood flow. It is considered a medical emergency because it can quickly result in life-threatening infection and death. Any cause of bowel ischemia, the earlier reversible form of injury, may ultimately lead to infarction if uncorrected. The causes of bowel ischemia or infarction include primary vascular causes and other causes of bowel obstruction.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.
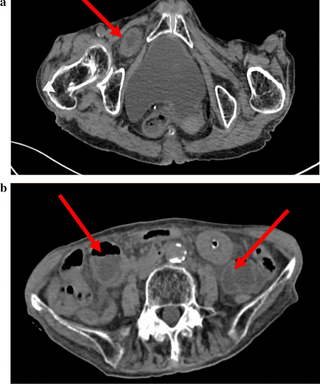
An obturator hernia is a rare type of hernia, encompassing 0.07-1% of all hernias, of the pelvic floor in which pelvic or abdominal contents protrudes through the obturator foramen. The obturator foramen is formed by a branch of the ischial as well as the pubic bone. The canal is typically 2-3 centimeters long and 1 centimeters wide, creating a space for pouches of pre-peritoneal fat.
An ileosigmoid knot or compound volvulus is an uncommon cause of intestinal blockage. The condition arises when ileum loops wrap around the bottom of a redundant sigmoid loop. In some countries in Africa, Asia, and the Middle East, the ileosigmoid knot is a well-known ailment; this condition is uncommon in the West.
Afferent loop syndrome is an uncommon side effect of gastric surgery. The afferent loop is made up of a segment of duodenum and/or proximal jejunum located upstream of a double-barrel gastrojejunostomy anastomosis. Abdominal pain and distension are signs of increased intraluminal pressure resulting from the accumulation of enteric secretions in the obstructed afferent loop.