Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver. The digestive system functions to move material through the GI tract via peristalsis, break down that material via digestion, absorb nutrients for use throughout the body, and remove waste from the body via defecation. Physicians who specialize in the medical specialty of gastroenterology are called gastroenterologists or sometimes GI doctors. Some of the most common conditions managed by gastroenterologists include gastroesophageal reflux disease, gastrointestinal bleeding, irritable bowel syndrome, inflammatory bowel disease (IBD) which includes Crohn's disease and ulcerative colitis, peptic ulcer disease, gallbladder and biliary tract disease, hepatitis, pancreatitis, colitis, colon polyps and cancer, nutritional problems, and many more.

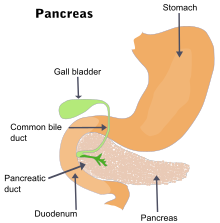
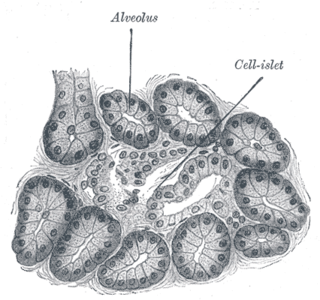
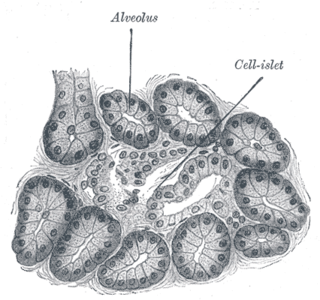
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

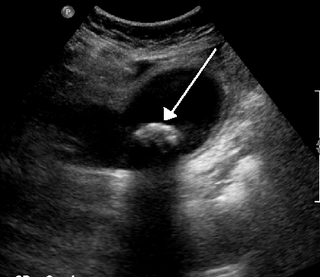
A gallstone is a stone formed within the gallbladder from precipitated bile components. The term cholelithiasis may refer to the presence of gallstones or to any disease caused by gallstones, and choledocholithiasis refers to the presence of migrated gallstones within bile ducts.
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks precede acute cholecystitis. The pain lasts longer in cholecystitis than in a typical gallbladder attack. Without appropriate treatment, recurrent episodes of cholecystitis are common. Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.

Abdominal pain, also known as a stomach ache, Is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; heavy alcohol use; systemic disease; trauma; and, in children, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis.

Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis. Tobacco smoke and alcohol misuse are two of the most frequently implicated causes, and the two risk factors are thought to have a synergistic effect with regards to the development of chronic pancreatitis. Chronic pancreatitis is a risk factor for the development of pancreatic cancer.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Common bile duct stone, also known as choledocholithiasis, is the presence of gallstones in the common bile duct (CBD). This condition can cause jaundice and liver cell damage. Treatments include choledocholithotomy and endoscopic retrograde cholangiopancreatography (ERCP).

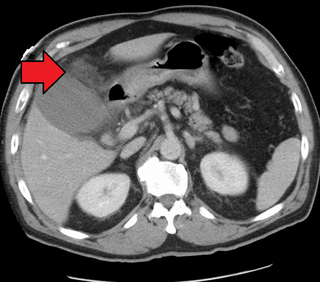
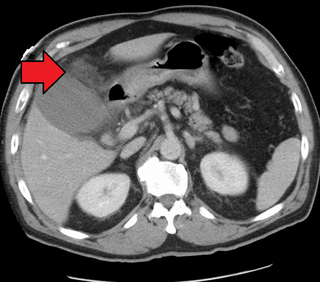
A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pseudocysts are like cysts, but lack epithelial or endothelial cells. Initial management consists of general supportive care. Symptoms and complications caused by pseudocysts require surgery. Computed tomography (CT) scans are used for initial imaging of cysts, and endoscopic ultrasounds are used in differentiating between cysts and pseudocysts. Endoscopic drainage is a popular and effective method of treating pseudocysts.

Pancreatic divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). In some cases, it may be detected intraoperatively. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.

Hereditary pancreatitis (HP) is an inflammation of the pancreas due to genetic causes. It was first described in 1952 by Comfort and Steinberg but it was not until 1996 that Whitcomb et al isolated the first responsible mutation in the trypsinogen gene (PRSS1) on the long arm of chromosome seven (7q35).

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.
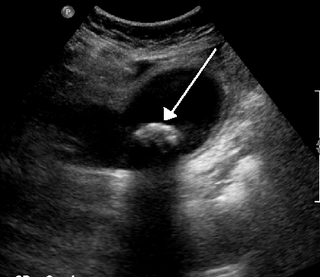
Biliary colic, also known as symptomatic cholelithiasis, a gallbladder attack or gallstone attack, is when a colic occurs due to a gallstone temporarily blocking the cystic duct. Typically, the pain is in the right upper part of the abdomen, and can be severe. Pain usually lasts from 15 minutes to a few hours. Often, it occurs after eating a heavy meal, or during the night. Repeated attacks are common. Cholecystokinin - a gastrointestinal hormone - plays a role in the colic, as following the consumption of fatty meals, the hormone triggers the gallbladder to contract, which may expel stones into the duct and temporarily block it until being successfully passed.

Gallbladder diseases are diseases involving the gallbladder and is closely linked to biliary disease, with the most common cause being gallstones (cholelithiasis).

The abdominopelvic cavity is a body cavity that consists of the abdominal cavity and the pelvic cavity. The upper portion is the abdominal cavity, and it contains the stomach, liver, pancreas, spleen, gallbladder, kidneys, small intestine, and most of the large intestine. The lower portion is the pelvic cavity, and it contains the urinary bladder, the rest of the large intestine, and the internal reproductive organs.
Canine pancreatitis is inflammation of the pancreas that can occur in two very different forms. Acute pancreatitis is sudden, while chronic pancreatitis is characterized by recurring or persistent form of pancreatic inflammation. Cases of both can be considered mild or severe.
Type 3c diabetes is diabetes that comes secondary to pancreatic diseases, involving the exocrine and digestive functions of the pancreas. It also occurs following surgical removal of the pancreas.