Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.

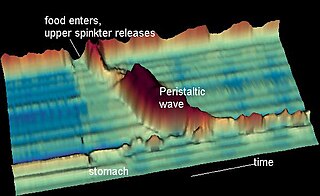
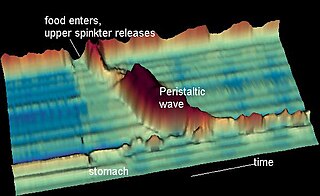
The esophagus or oesophagus, colloquially known also as the food pipe, food tube, or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid into the esophagus. It is the major symptom of gastroesophageal reflux disease (GERD).
An esophageal motility disorder (EMD) is any medical disorder resulting from dysfunction of the coordinated movement of esophagus, which causes dysphagia.

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is a chronic upper gastrointestinal disease in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".
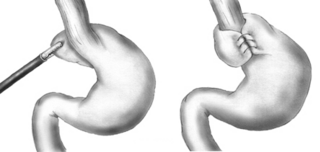
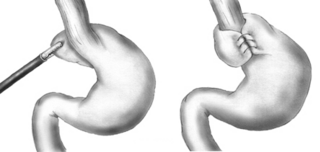
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.
Esophageal webs are thin membranes occurring anywhere along the esophagus.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.

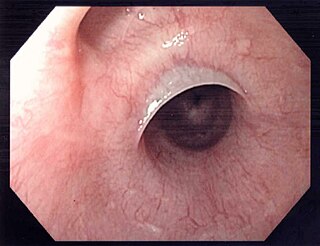
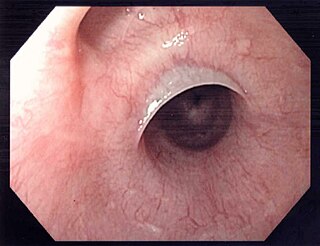
A Schatzki ring or Schatzki–Gary ring is a narrowing of the lower esophagus that can cause difficulty swallowing (dysphagia). The narrowing is caused by a ring of mucosal tissue or muscular tissue. A Schatzki ring is a specific type of "esophageal ring", and Schatzki rings are further subdivided into those above the esophagus/stomach junction, and those found at the squamocolumnar junction in the lower esophagus.
Esophageal spasm is a disorder of motility of the esophagus.
Nutcracker esophagus, jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, with both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.

Diffuse esophageal spasm (DES), also known as distal esophageal spasm, is a condition characterized by uncoordinated contractions of the esophagus, which may cause difficulty swallowing (dysphagia) or regurgitation. In some cases, it may cause symptoms such as chest pain, similar to heart disease. In many cases, the cause of DES remains unknown.

A benign esophageal stricture, or peptic stricture, is a narrowing or tightening of the esophagus that causes swallowing difficulties.

Lymphocytic esophagitis is a rare and poorly understood medical disorder involving inflammation in the esophagus. The disease is named from the primary inflammatory process, wherein lymphocytes are seen within the esophageal mucosa. Symptoms of the condition include difficulty swallowing, heartburn and food bolus obstruction. The condition was first described in 2006 by Rubio and colleagues. Initial reports questioned whether this was a true medical disorder, or whether the inflammation was secondary to another condition, such as gastroesophageal reflux disease.
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractory symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.