Irritation, in biology and physiology, is a state of inflammation or painful reaction to allergy or cell-lining damage. A stimulus or agent which induces the state of irritation is an irritant. Irritants are typically thought of as chemical agents but mechanical, thermal (heat), and radiative stimuli can also be irritants. Irritation also has non-clinical usages referring to bothersome physical or psychological pain or discomfort.

Tinea cruris, also known as jock itch, is a common type of contagious, superficial fungal infection of the groin and buttocks region, which occurs predominantly but not exclusively in men and in hot-humid climates.

Itch is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.

Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus. Signs and symptoms often include itching, scaling, cracking and redness. In rare cases the skin may blister. Athlete's foot fungus may infect any part of the foot, but most often grows between the toes. The next most common area is the bottom of the foot. The same fungus may also affect the nails or the hands. It is a member of the group of diseases known as tinea.
Antipruritics, abirritants, or anti-itch drugs, are medications that inhibit the itching often associated with sunburns, allergic reactions, eczema, psoriasis, chickenpox, fungal infections, insect bites and stings like those from mosquitoes, fleas, and mites, and contact dermatitis and urticaria caused by plants such as poison ivy or stinging nettle. It can also be caused by chronic kidney disease and related conditions.

Cutaneous larva migrans is a skin disease in humans, caused by the larvae of various nematode parasites of the hookworm family (Ancylostomatidae). The parasites live in the intestines of dogs, cats, and wild animals; they should not be confused with other members of the hookworm family for which humans are definitive hosts, namely Ancylostoma duodenale and Necator americanus.
Aquagenic pruritus is a skin condition characterized by the development of severe, intense, prickling-like epidermal itching without observable skin lesions and evoked by contact with water.
Vulvitis is inflammation of the vulva, the external female mammalian genitalia that include the labia majora, labia minora, clitoris, and introitus. It may co-occur as vulvovaginitis with vaginitis, inflammation of the vagina, and may have infectious or non-infectious causes. The warm and moist conditions of the vulva make it easily affected. Vulvitis is prone to occur in any female especially those who have certain sensitivities, infections, allergies, or diseases that make them likely to have vulvitis. Postmenopausal women and prepubescent girls are more prone to be affected by it, as compared to women in their menstruation period. It is so because they have low estrogen levels which makes their vulvar tissue thin and dry. Women having diabetes are also prone to be affected by vulvitis due to the high sugar content in their cells, increasing their vulnerability. Vulvitis is not a disease, it is just an inflammation caused by an infection, allergy or injury. Vulvitis may also be symptom of any sexually transmitted infection or a fungal infection.
Proctitis is an inflammation of the anus and the lining of the rectum, affecting only the last 6 inches of the rectum.

Anal fistula is a chronic abnormal communication between the anal canal and the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.

Clobetasone (INN) is a corticosteroid used in dermatology, for treating such skin inflammation as seen in eczema, psoriasis and other forms of dermatitis, and ophthalmology. Topical clobetasone butyrate has shown minimal suppression of the hypothalamic–pituitary–adrenal axis.

Notalgia paresthetica or Notalgia paraesthetica (NP) (also known as "Hereditary localized pruritus", "Posterior pigmented pruritic patch", and "subscapular pruritus") is a chronic sensory neuropathy. Notalgia paresthetica is a common localized itch, affecting mainly the area between the shoulder blades (especially the T2–T6 dermatomes) but occasionally with a more widespread distribution, involving the shoulders, back, and upper chest. The characteristic symptom is pruritus (itch or sensation that makes a person want to scratch) on the back, usually on the left hand side below the shoulder blade (mid to upper back). It is occasionally accompanied by pain, paresthesia (pins and needles), or hyperesthesia (unusual or pathologically increased sensitivity of the skin to sensory stimuli, such as pain, heat, cold, or touch), which results in a well circumscribed hyperpigmentation of a skin patch in the affected area.

In humans, the anus is the external opening of the rectum located inside the intergluteal cleft. Two sphincters control the exit of feces from the body during an act of defecation, which is the primary function of the anus. These are the internal anal sphincter and the external anal sphincter, which are circular muscles that normally maintain constriction of the orifice and which relaxes as required by normal physiological functioning. The inner sphincter is involuntary and the outer is voluntary. Above the anus is the perineum, which is also located beneath the vulva or scrotum.
Brachioradial pruritus is an intense itching sensation of the arm usually between the wrist and elbow of either or both arms. The itch can be so intense that affected individuals will scratch their own skin to a bleeding condition.
Pruritus vulvae is itchiness of the vulva, which is the counterpart of pruritus scroti, and may have many different causes. Patch testing may be used to diagnose the cause.
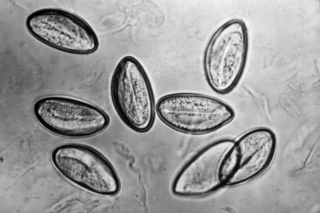
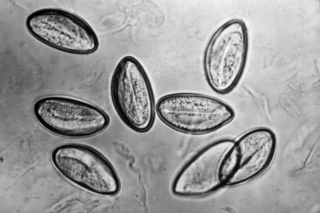
Pinworm infection, also known as enterobiasis, is a human parasitic disease caused by the pinworm, Enterobius vermicularis. The most common symptom is itching in the anal area. The period of time from swallowing eggs to the appearance of new eggs around the anus is 4 to 8 weeks. Some people who are infected do not have symptoms.
Senile pruritus is one of the most common conditions in the elderly or people over 65 years of age with an emerging itch that may be accompanied with changes in temperature and textural characteristics. In the elderly, xerosis, is the most common cause for an itch due to the degradation of the skin barrier over time. However, the cause of senile pruritus is not clearly known. Diagnosis is based on an elimination criteria during a full body examination that can be done by either a dermatologist or non-dermatologist physician.
Perianal cellulitis, also known as perianitis or perianal streptococcal dermatitis, is a bacterial infection affecting the lower layers of the skin (cellulitis) around the anus. It presents as bright redness in the skin and can be accompanied by pain, difficulty defecating, itching, and bleeding. This disease is considered a complicated skin and soft tissue infection (cSSTI) because of the involvement of the deeper soft tissues.
Rectal discharge is intermittent or continuous expression of liquid from the anus. Normal rectal mucus is needed for proper excretion of waste. Otherwise, this is closely related to types of fecal incontinence but the term rectal discharge does not necessarily imply degrees of incontinence. Types of fecal incontinence that produce a liquid leakage could be thought of as a type of rectal discharge.
Topical antifungaldrugs are used to treat fungal infections on the skin, scalp, nails, vagina or inside the mouth. These medications come as creams, gels, lotions, ointments, powders, shampoos, tinctures and sprays. Most antifungal drugs induce fungal cell death by destroying the cell wall of the fungus. These drugs inhibit the production of ergosterol, which is a fundamental component of the fungal cell membrane and wall.