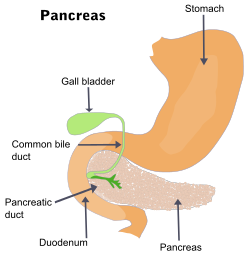
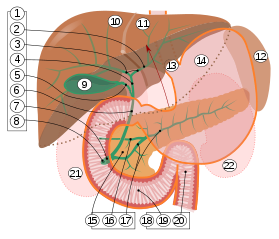
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In mammals it may be the principal site for iron absorption. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.

In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although the structure and position of the gallbladder can vary significantly among animal species. It receives bile, produced by the liver, via the common hepatic duct, and stores it. The bile is then released via the common bile duct into the duodenum, where the bile helps in the digestion of fats.

A bile duct is any of a number of long tube-like structures that carry bile, and is present in most vertebrates. The bile duct is separated into three main parts: the fundus (superior), the body (middle), and the neck (inferior).

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.

The bile duct is a part of the biliary tract. It is formed by the union of the common hepatic duct and cystic duct. It ends by uniting with the pancreatic duct to form the hepatopancreatic ampulla. It possesses its own sphincter to enable regulation of bile flow.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.

Common bile duct stone, also known as choledocholithiasis, is the presence of gallstones in the common bile duct (CBD). This condition can cause jaundice and liver cell damage. Treatments include choledocholithotomy and endoscopic retrograde cholangiopancreatography (ERCP).

The ampulla of Vater, hepatopancreatic ampulla or hepatopancreatic duct is the common duct that is usually formed by a union of the common bile duct and the pancreatic duct within the wall of the duodenum. This common duct usually features a dilation ("ampulla"). The common duct then opens medially into the descending part of the duodenum at the major duodenal papilla. The common duct usually measures 2-10mm in length.

Pancreas divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). In some cases, it may be detected intraoperatively. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.

The major duodenal papilla is a rounded projection in the duodenum into which the common bile duct and pancreatic duct drain. The major duodenal papilla is, in most people, the primary mechanism for the secretion of bile and other enzymes that facilitate digestion.

The biliary tract refers to the liver, gallbladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and conjugated bilirubin. Some components are synthesized by hepatocytes ; the rest are extracted from the blood by the liver.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.
The minor duodenal papilla is the opening of the accessory pancreatic duct into the descending second section of the duodenum.

Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi: functional biliary sphincter of Oddi and functional pancreatic sphincter of Oddi disorder. The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum. The pathogenesis of this condition is recognized to encompass stenosis or dyskinesia of the sphincter of Oddi ; consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition. Both stenosis and dyskinesia can obstruct flow through the sphincter of Oddi and can therefore cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.

The sphincter of Oddi, abbreviated as SO, is a muscular valve that in some animals, including humans, controls the flow of bile and pancreatic juice out of the gallbladder and pancreas respectively through the ampulla of Vater into the second part of the duodenum. It is named after Ruggero Oddi.

Choledochoduodenostomy (CDD) is a surgical procedure to create an anastomosis, a surgical connection, between the common bile duct (CBD) and an alternative portion of the duodenum. In healthy individuals, the CBD meets the pancreatic duct at the ampulla of Vater, which drains via the major duodenal papilla to the second part of duodenum. In cases of benign conditions such as narrowing of the distal CBD or recurrent CBD stones, performing a CDD provides the diseased patient with CBD drainage and decompression. A side-to-side anastomosis is usually performed.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).