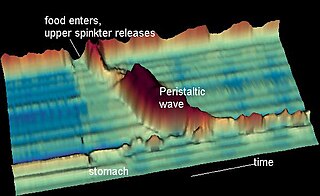
The esophagus or oesophagus, non-technically known also as the food pipe or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is one of the upper gastrointestinal chronic diseases where stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. On the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.
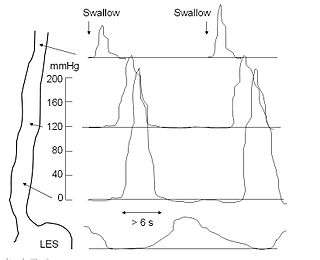
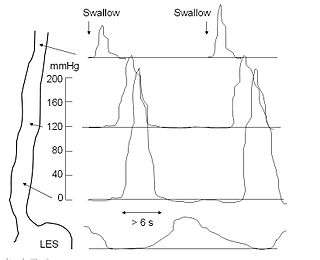
An esophageal motility study (EMS) or esophageal manometry is a test to assess motor function of the upper esophageal sphincter (UES), esophageal body and lower esophageal sphincter (LES).

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.
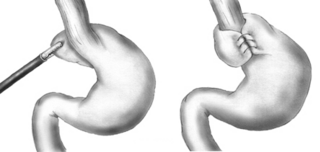
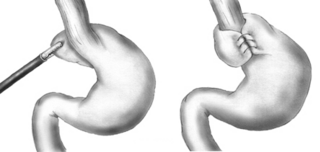
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Esophagectomy or oesophagectomy is the surgical removal of all or parts of the esophagus.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
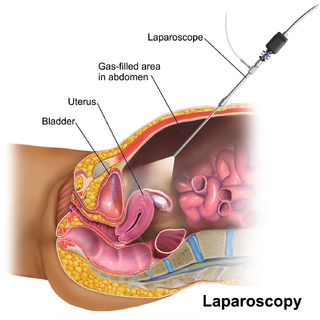
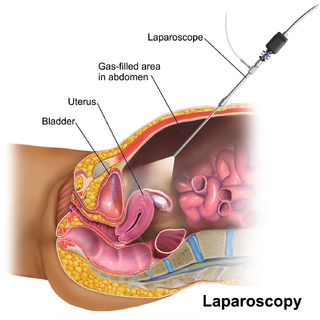
Laparoscopic hernia repair is the repair of a hiatal hernia using a laparoscope, which is a tiny telescope-like instrument. A hiatal hernia is the protrusion of an organ through its wall or cavity. There are several different methods that can be used when performing this procedure. Among them are the Nissen Fundoplication and the general laparoscopic hernia repair.
Stretta is a minimally invasive endoscopic procedure for the treatment of gastroesophageal reflux disease (GERD) that delivers radiofrequency energy in the form of electromagnetic waves through electrodes at the end of a catheter to the lower esophageal sphincter (LES) and the gastric cardia – the region of the stomach just below the LES. The energy heats the tissue, ultimately causing it to swell and stiffen; the way this works was not understood as of 2015, but it was thought that perhaps the heat causes local inflammation, collagen deposition and muscular thickening of the LES and that it may disrupt the nerves there.
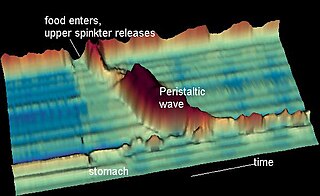
Nutcracker esophagus, Jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, to both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.
Pyloromyotomy is a surgical procedure in which a portion of the muscle fibers of the pyloric muscle are cut. This is typically done in cases where the contents from the stomach are inappropriately stopped by the pyloric muscle, causing the stomach contents to build up in the stomach and unable to be appropriately digested. The procedure is typically performed in cases of "hypertrophic pyloric stenosis" in young children. In most cases, the procedure can be performed with either an open approach or a laparoscopic approach and the patients typically have good outcomes with minimal complications.
Norman Rupert Barrett was an Australian-born British thoracic surgeon who is widely yet mistakenly remembered for describing what became known as Barrett's oesophagus.
A Collis gastroplasty is a surgical procedure performed when the surgeon desires to create a Nissen fundoplication, but the portion of esophagus inferior to the diaphragm is too short. Thus, there is not enough esophagus to wrap. A vertical incision is made in the stomach parallel to the left border of the esophagus. This effectively lengthens the esophagus. The stomach fundus can then be wrapped around the neo-esophagus, thus reducing reflux of stomach acid into the esophagus.

Rudolph Nissen was a surgeon who chaired surgery departments in Turkey, the United States and Switzerland. The Nissen fundoplication, a surgical procedure for the treatment of gastroesophageal reflux disease, is named after him.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractor symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.