Related Research Articles

Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems. A special case is that of congenital amputation, a congenital disorder, where fetal limbs have been cut off by constrictive bands. In some countries, judicial amputation is currently used to punish people who commit crimes. Amputation has also been used as a tactic in war and acts of terrorism; it may also occur as a war injury. In some cultures and religions, minor amputations or mutilations are considered a ritual accomplishment. When done by a person, the person executing the amputation is an amputator. The oldest evidence of this practice comes from a skeleton found buried in Liang Tebo cave, East Kalimantan, Indonesian Borneo dating back to at least 31,000 years ago, where it was done when the amputee was a young child.

Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the urinary system and the reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.

Surgery is a medical specialty that uses manual and instrumental techniques to diagnose or treat pathological conditions, to alter bodily functions, to reconstruct or improve aesthetics and appearance, or to remove unwanted tissues or foreign bodies. The subject receiving the surgery is typically a person, but can also be a non-human animal.
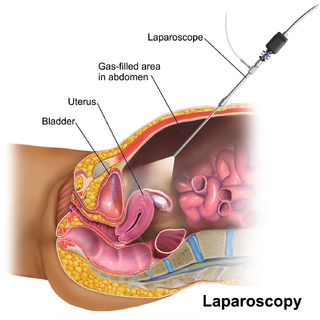
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.

A bone tumor is an abnormal growth of tissue in bone, traditionally classified as noncancerous (benign) or cancerous (malignant). Cancerous bone tumors usually originate from a cancer in another part of the body such as from lung, breast, thyroid, kidney and prostate. There may be a lump, pain, or neurological signs from pressure. A bone tumor might present with a pathologic fracture. Other symptoms may include fatigue, fever, weight loss, anemia and nausea. Sometimes there are no symptoms and the tumour is found when investigating another problem.

Battlefield medicine, also called field surgery and later combat casualty care, is the treatment of wounded combatants and non-combatants in or near an area of combat. Civilian medicine has been greatly advanced by procedures that were first developed to treat the wounds inflicted during combat. With the advent of advanced procedures and medical technology, even polytrauma can be survivable in modern wars. Battlefield medicine is a category of military medicine.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.

Minimally invasive procedures encompass surgical techniques that limit the size of incisions needed, thereby reducing wound healing time, associated pain, and risk of infection. Surgery by definition is invasive, and many operations requiring incisions of some size are referred to as open surgery. Incisions made during open surgery can sometimes leave large wounds that may be painful and take a long time to heal. Advancements in medical technologies have enabled the development and regular use of minimally invasive procedures. For example, endovascular aneurysm repair, a minimally invasive surgery, has become the most common method of repairing abdominal aortic aneurysms in the US as of 2003. The procedure involves much smaller incisions than the corresponding open surgery procedure of open aortic surgery.

Hemipelvectomy, also known as a pelvic resection, is a surgical procedure that involves the removal of part of the pelvic girdle. This procedure is most commonly performed to treat oncologic conditions of the pelvis. Hemipelvectomy can be further classified as internal and external hemipelvectomy. An internal hemipelvectomy is a limb-sparing procedure where the innominate bone is resected while preserving the ipsilateral limb. An external hemipelvectomy involves the resection of the innominate bone plus amputation of the ipsilateral limb.
In anatomy, a stoma is any opening in the body. For example, a mouth, a nose, and an anus are natural stomata. Any hollow organ can be manipulated into an artificial stoma as necessary. This includes the esophagus, stomach, duodenum, ileum, colon, pleural cavity, ureters, urinary bladder, and renal pelvis. Such a stoma may be permanent or temporary.
In medicine, the ileal pouch–anal anastomosis (IPAA), also known as restorative proctocolectomy (RPC), ileal-anal reservoir (IAR), an ileo-anal pouch, ileal-anal pullthrough, or sometimes referred to as a J-pouch, S-pouch, W-pouch, or a pelvic pouch, is an anastomosis of a reservoir pouch made from ileum to the anus, bypassing the former site of the colon in cases where the colon and rectum have been removed. The pouch retains and restores functionality of the anus, with stools passed under voluntary control of the person, preventing fecal incontinence and serving as an alternative to a total proctocolectomy with ileostomy.

Pelvic exenteration is a radical surgical treatment that removes all organs from a person's pelvic cavity. It is used to treat certain advanced or recurrent cancers. The urinary bladder, urethra, rectum, and anus are removed. In women, the vagina, cervix, uterus, Fallopian tubes, ovaries and, in some cases, the vulva are removed. In men, the prostate is removed. The procedure leaves the person with a permanent colostomy and urinary diversion.

Vaginectomy is a surgery to remove all or part of the vagina. It is one form of treatment for individuals with vaginal cancer or rectal cancer that is used to remove tissue with cancerous cells. It can also be used in gender-affirming surgery. Some people born with a vagina who identify as trans men or as nonbinary may choose vaginectomy in conjunction with other surgeries to make the clitoris more penis-like (metoidioplasty), construct of a full-size penis (phalloplasty), or create a relatively smooth, featureless genital area.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, sports-related injuries, and are notably common among the elderly who experience falls.
Rotationplasty, commonly known as a Van Nes rotation or Borggreve rotation, is a type of autograft wherein a portion of a limb is removed, while the remaining limb below the involved portion is rotated and reattached. This procedure is used when a portion of an extremity is injured or involved with a disease, such as cancer.
An exploratory laparotomy is a general surgical operation where the abdomen is opened and the abdominal organs are examined for injury or disease. It is the standard of care in various blunt and penetrating trauma situations in which there may be life-threatening internal injuries. It is also used in certain diagnostic situations, in which the operation is undertaken in search of a unifying cause for multiple signs and symptoms of disease, and in the staging of some cancers.
Limb-sparing techniques, also known as limb-saving or limb-salvage techniques, are performed in order to preserve the look and function of limbs. Limb-sparing techniques are used to preserve limbs affected by trauma, arthritis, cancers such as high-grade bone sarcomas, and vascular conditions such as diabetic foot ulcers. As the techniques for chemotherapy, radiation, and diagnostic modalities improve, there has been a trend toward limb-sparing procedures to avoid amputation, which has been associated with a lower 5-year survival rate and cost-effectiveness compared to limb salvage in the long-run. There are many different types of limb-sparing techniques, including arthrodesis, arthroplasty, endoprosthetic reconstruction, various types of implants, rotationplasty, osseointegration limb replacement, fasciotomy, and revascularization.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.

A resuscitative thoracotomy (sometimes referred to as an emergency department thoracotomy (EDT), trauma thoracotomy or, colloquially, as "cracking the chest") is a thoracotomy performed to aid in the resuscitation of a major trauma patient who has sustained severe thoracic or abdominal trauma. The procedure allows immediate direct access to the thoracic cavity, permitting rescuers to control hemorrhage, relieve cardiac tamponade, repair or control major injuries to the heart, lungs or thoracic vasculature, and perform direct cardiac massage or defibrillation. The procedure is rarely performed and is a procedure of last resort.

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a minimally invasive procedure performed during resuscitation of critically injured trauma patients. Originally developed as a less invasive alternative to emergency thoracotomy with aortic cross clamping, REBOA is performed to gain rapid control of non-compressible truncal or junctional hemorrhage. REBOA is performed first by achieving access to the common femoral artery (CFA) and advancing a catheter within the aorta. Upon successful catheter placement, an occluding balloon may be inflated either within the descending thoracic aorta or infrarenal abdominal aorta. REBOA stanches downstream hemorrhage and improves cardiac index, cerebral perfusion, and coronary perfusion. Although REBOA does not eliminate the need for definitive hemorrhage control, it may serve as a temporizing measure during initial resuscitation. Despite the benefits of REBOA, there are significant local and systemic ischemic risks. Establishing standardized REBOA procedural indications and mitigating the risk of ischemic injury are topics of ongoing investigation. Although this technique has been successfully deployed in adult patients, it has not yet been studied in children.
References
- 1 2 3 Ferrara, Bernard E. (December 1990). "Hemicorporectomy: A Collective Review". Journal of Surgical Oncology. 45 (4): 270–278. doi:10.1002/jso.2930450412. PMID 2250478. S2CID 35307193.
- 1 2 Shields, Richard K.; Dudley-Javoroski, Shauna (March 2003). "Musculoskeletal Deterioration and Hemicorporectomy After Spinal Cord Injury". Physical Therapy. 83 (3): 263–275. doi:10.1093/ptj/83.3.263. PMC 4042312 . PMID 12620090. Archived from the original on June 27, 2004.
- ↑ Porter-Romatowski, Tracy L.; Deckert, M. M. Johanna (April 1998). "Hemicorporectomy: a case study from a physical therapy perspective". Archives of Physical Medicine and Rehabilitation. 79 (4): 464–468. doi:10.1016/S0003-9993(98)90152-6. PMID 9552117.
- ↑ Janis, Jeffrey E; Ahmad, Jamil; Lemmon, Joshua A; Barnett Jr, Carlton C; Morrill, Kevin C; McClelland, Robert N (October 2009). "A 25-year experience with hemicorporectomy for terminal pelvic osteomyelitis". Plastic and Reconstructive Surgery. 124 (4): 1165–76. doi:10.1097/PRS.0b013e3181b61169. PMID 19935300. S2CID 19312510.
- ↑ Weaver, Jane; Flynn, Michael (Feb 2000). "Hemicorporectomy". Journal of Surgical Oncology. 73 (2): 117–24. doi:10.1002/(SICI)1096-9098(200002)73:2<117::AID-JSO12>3.0.CO;2-C. PMID 10694650.
- ↑ Aust, JB; Page, CP (Dec 1985). "Hemicorporectomy". Journal of Surgical Oncology. 30 (4): 226–30. doi:10.1002/jso.2930300408. PMID 4079439. S2CID 221890435.
- ↑ Terz, J. J.; Schaffner, M. J.; Goodkin, R.; Beatty, J. D.; Razor, B.; Weliky, A.; Shimabukuro, C. (June 1990). "Translumbar amputation". Cancer. 65 (12): 2668–2675. doi: 10.1002/1097-0142(19900615)65:12<2668::AID-CNCR2820651212>3.0.CO;2-I . PMID 2340466.
- ↑ Sherwood, Dave; Deakin, Charles (2020). Resuscitation Policy and Recognition of Life Extinct (PDF) (7th ed.). Oxfordshire, England: South Central Ambulance Service NHS Foundation Trust. pp. 16, 46. Archived (PDF) from the original on 2023-05-10. Retrieved 21 April 2022.
- ↑ Hopson LR, Hirsh E, Delgado J, Domeier RM, McSwain NE, Krohmer J (January 2003). "Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: joint position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma". Journal of the American College of Surgeons. 196 (1): 106–112. doi:10.1016/S1072-7515(02)01668-X. PMID 12517561.
- ↑ Walker SJ, Johnson RH (1989). "Traumatic hemisomato-tmesis: a case report and review of the literature". Arch Emerg Med. 6 (1): 66–9. doi:10.1136/emj.6.1.66. PMC 1285562 . PMID 2653349.
- ↑ "Great Falls teen, amputated from the waist down, inspires millions". KRTV. 2020-11-26. Retrieved 2022-07-12.
- ↑ Loren’s Accident (previously titled: "Loren's Story: Viral TikTok Story Time") , retrieved 2022-07-12
- ↑ "Sabia and Loren - YouTube". www.youtube.com. Retrieved 2022-07-12.