Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Bleeding, hemorrhage, haemorrhage or blood loss is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a puncture in the skin. Hypovolemia is a massive decrease in blood volume, and death by excessive loss of blood is referred to as exsanguination. Typically, a healthy person can endure a loss of 10–15% of the total blood volume without serious medical difficulties. The stopping or controlling of bleeding is called hemostasis and is an important part of both first aid and surgery.

In physiology, dehydration is a lack of total body water, with an accompanying disruption of metabolic processes. It occurs when free water loss exceeds free water intake, usually due to exercise, disease, or high environmental temperature. Mild dehydration can also be caused by immersion diuresis, which may increase risk of decompression sickness in divers.
Iron poisoning typically occurs from ingestion of excess iron that results in acute toxicity. Mild symptoms which occur within hours include vomiting, diarrhea, abdominal pain, and drowsiness. In more severe cases, symptoms can include tachypnea, low blood pressure, seizures, or coma. If left untreated, iron poisoning can lead to multi-organ failure resulting in permanent organ damage or death.

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.
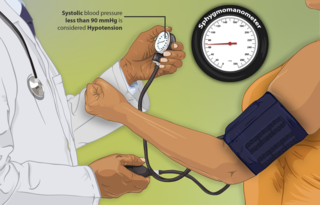
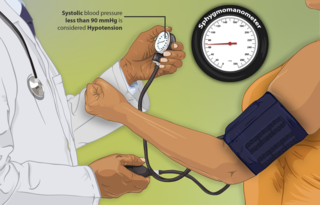
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Thirst is the craving for potable fluids, resulting in the basic instinct of animals to drink. It is an essential mechanism involved in fluid balance. It arises from a lack of fluids or an increase in the concentration of certain osmolites, such as sodium. If the water volume of the body falls below a certain threshold or the osmolite concentration becomes too high, structures in the brain detect changes in blood constituents and signal thirst.
Hematemesis is the vomiting of blood. It can be confused with hemoptysis or epistaxis (nosebleed), which are more common. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum. It may be caused by ulcers, tumors of the stomach or esophagus, varices, prolonged and vigorous retching, gastroenteritis, ingested blood, or certain drugs.

Internal bleeding is a loss of blood from a blood vessel that collects inside the body, and is not usually visible from the outside. It can be a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding. Severe internal bleeding into the chest, abdomen, pelvis, or thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly. Internal bleeding is a medical emergency and should be treated immediately by medical professionals.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.
Oliguria or hypouresis is the low output of urine specifically more than 80 ml/day but less than 400ml/day. The decreased output of urine may be a sign of dehydration, kidney failure, hypovolemic shock, hyperosmolar hyperglycemic nonketotic syndrome (HHNS), multiple organ dysfunction syndrome, urinary obstruction/urinary retention, diabetic ketoacidosis (DKA), pre-eclampsia, and urinary tract infections, among other conditions.

Neurogenic shock is a distributive type of shock resulting in hypotension, often with bradycardia, caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nervous system, such as spinal cord injury and traumatic brain injury. Low blood pressure occurs due to decreased systemic vascular resistance resulting from loss of sympathetic tone, which in turn causes blood pooling within the extremities rather than being available to circulate throughout the body. The slowed heart rate results from a vagal response unopposed by a sympathetic nervous system (SNS) response. Such cardiovascular instability is exacerbated by hypoxia, or treatment with endotracheal or endobronchial suction used to prevent pulmonary aspiration.
Lightheadedness is a common and typically unpleasant sensation of dizziness or a feeling that one may faint. The sensation of lightheadedness can be short-lived, prolonged, or, rarely, recurring. In addition to dizziness, the individual may feel as though their head is weightless. The individual may also feel as though the room is "spinning" or moving (vertigo). Most causes of lightheadedness are not serious and either cure themselves quickly or are easily treated.
Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.
End organ damage is severe impairment of major body organs due to high blood pressure or states of low blood pressure or low blood volume. This can present as a heart attack or heart failure, pulmonary edema, neurologic deficits including a stroke, or acute kidney failure.

An amniotic fluid embolism (AFE) is a life-threatening childbirth (obstetric) emergency in which amniotic fluid enters the blood stream of the mother, triggering a serious reaction which results in cardiorespiratory collapse and massive bleeding (coagulopathy). The rate at which it occurs is 1 instance per 20,000 births and it comprises 10% of all maternal deaths.
In medicine, intravascular volume status refers to the volume of blood in a patient's circulatory system, and is essentially the blood plasma component of the overall volume status of the body, which otherwise includes both intracellular fluid and extracellular fluid. Still, the intravascular component is usually of primary interest, and volume status is sometimes used synonymously with intravascular volume status.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and tension pneumothorax. These are all life-threatening. Symptoms may include shortness of breath, weakness, or altered mental status. Low blood pressure and tachycardia are often seen in shock. Other symptoms depend on the underlying cause.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50 mmHg or systolic blood pressure of less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury, some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding are thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.