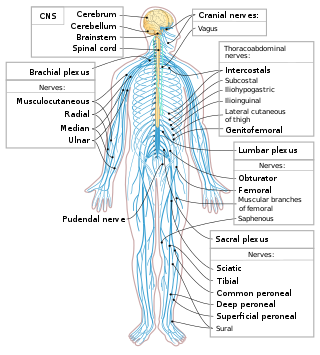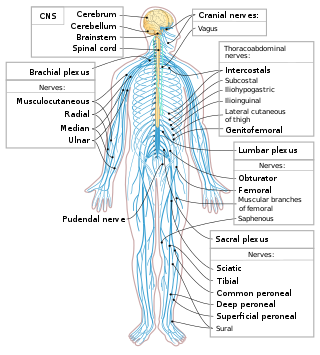
The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of nerves and ganglia, which lie outside the brain and the spinal cord. The main function of the PNS is to connect the CNS to the limbs and organs, essentially serving as a relay between the brain and spinal cord and the rest of the body. Unlike the CNS, the PNS is not protected by the vertebral column and skull, or by the blood–brain barrier, which leaves it exposed to toxins.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.
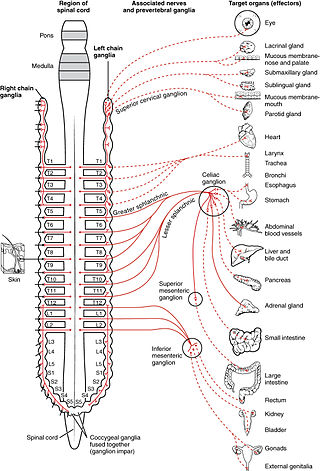
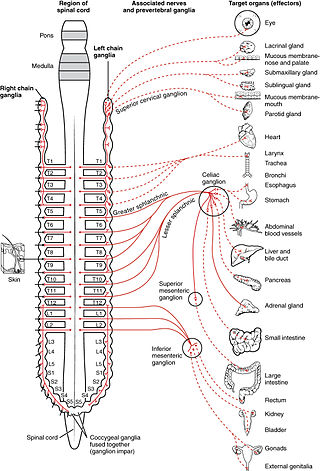
The sympathetic nervous system (SNS) is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
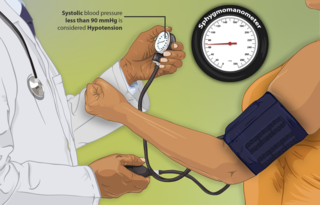
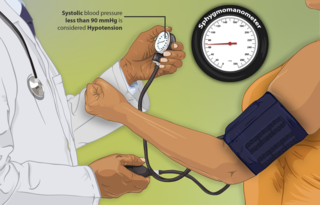
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Hypovolemia, also known as volume depletion or volume contraction, is a state of abnormally low extracellular fluid in the body. This may be due to either a loss of both salt and water or a decrease in blood volume. Hypovolemia refers to the loss of extracellular fluid and should not be confused with dehydration.

Respiratory arrest is a medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete, with a total loss of sensation and muscle function at lower sacral segments, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord up to the Sacral S4-5 spinal cord segments. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis, including bowel or bladder incontinence. Long term outcomes also range widely, from full recovery to permanent tetraplegia or paraplegia. Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.
Cushing reflex is a physiological nervous system response to increased intracranial pressure (ICP) that results in Cushing's triad of increased blood pressure, irregular breathing, and bradycardia. It is usually seen in the terminal stages of acute head injury and may indicate imminent brain herniation. It can also be seen after the intravenous administration of epinephrine and similar drugs. It was first described in detail by American neurosurgeon Harvey Cushing in 1901.

Traumatic cardiac arrest (TCA) is a condition in which the heart has ceased to beat due to blunt or penetrating trauma, such as a stab wound to the thoracic area. It is a medical emergency which will always result in death without prompt advanced medical care. Even with prompt medical intervention, survival without neurological complications is rare. In recent years, protocols have been proposed to improve survival rate in patients with traumatic cardiac arrest, though the variable causes of this condition as well as many coexisting injuries can make these protocols difficult to standardize. Traumatic cardiac arrest is a complex form of cardiac arrest often derailing from advanced cardiac life support in the sense that the emergency team must first establish the cause of the traumatic arrest and reverse these effects, for example hypovolemia and haemorrhagic shock due to a penetrating injury.

The baroreflex orbaroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. Their function is to sense pressure changes by responding to change in the tension of the arterial wall The baroreflex can begin to act in less than the duration of a cardiac cycle and thus baroreflex adjustments are key factors in dealing with postural hypotension, the tendency for blood pressure to decrease on standing due to gravity.
Spinal shock was first explored by Whytt in 1750 as a loss of sensation accompanied by motor paralysis with initial loss but gradual recovery of reflexes, following a spinal cord injury (SCI) – most often a complete transection. Reflexes in the spinal cord below the level of injury are depressed (hyporeflexia) or absent (areflexia), while those above the level of the injury remain unaffected. The 'shock' in spinal shock does not refer to circulatory collapse, and should not be confused with neurogenic shock, which is life-threatening. The term “spinal shock” was introduced more than 150 years ago in an attempt to distinguish arterial hypotension due to a hemorrhagic source from arterial hypotension due to loss of sympathetic tone resulting from spinal cord injury. Whytt, however, may have discussed the same phenomenon a century earlier, although no descriptive term was assigned.
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. It is one of four categories of shock, a condition where there is not enough oxygen-carrying blood to meet the metabolic needs of the cells which make up the body's tissues and organs. Distributive shock is different from the other three categories of shock in that it occurs even though the output of the heart is at or above a normal level. The most common cause is sepsis leading to a type of distributive shock called septic shock, a condition that can be fatal.
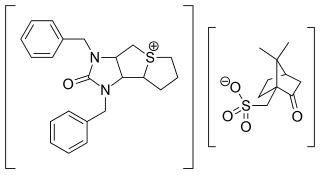
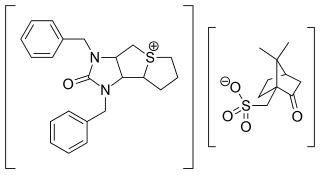
Trimetaphan camsilate (INN) or trimethaphan camsylate (USAN), trade name Arfonad, is a drug that counteracts cholinergic transmission at the ganglion type of nicotinic receptors of the autonomic ganglia and therefore blocks both the sympathetic nervous system and the parasympathetic nervous system. It acts as a non-depolarizing competitive antagonist at the nicotinic acetylcholine receptor, is short-acting, and is given intravenously.
Autonomic dysreflexia (AD) is a potentially fatal medical emergency classically characterized by uncontrolled hypertension and cardiac arrhythmia. AD occurs most often in individuals with spinal cord injuries with lesions at or above the T6 spinal cord level, although it has been reported in patients with lesions as low as T10. Guillain–Barré syndrome may also cause autonomic dysreflexia.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
The Bezold–Jarisch reflex involves a variety of cardiovascular and neurological processes which cause hypopnea, hypotension and bradycardia in response to noxious stimuli detected in the cardiac ventricles. The reflex is named after Albert von Bezold and Adolf Jarisch Junior. The significance of the discovery is that it was the first recognition of a chemical (non-mechanical) reflex.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50 mmHg or systolic blood pressure of less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury, some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding are thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
Vasodilatory shock, vasogenic shock, or vasoplegic shock is a medical emergency belonging to shock along with cardiogenic shock, septic shock, allergen-induced shock and hypovolemic shock. When the blood vessels suddenly relax, it results in vasodilation. In vasodilatory shock, the blood vessels are too relaxed leading to extreme vasodilation and blood pressure drops and blood flow becomes very low. Without enough blood pressure, blood and oxygen won't be pushed to reach the body's organs. If vasodilatory shock lasts more than a few minutes, the lack of oxygen starts to damage the body's organs. Vasodilatory shock like other types of shock should be treated quickly, otherwise it can cause permanent organ damage or death as a result of multiple organ dysfunction.