Related Research Articles

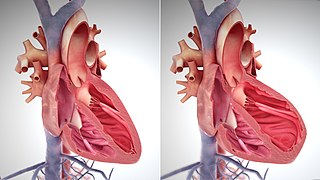
The heart is a muscular organ found in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as carbon dioxide to the lungs. In humans, the heart is approximately the size of a closed fist and is located between the lungs, in the middle compartment of the chest, called the mediastinum.
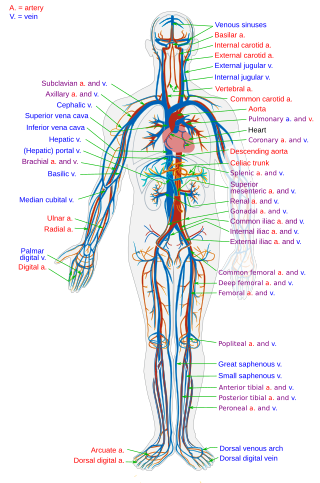
The circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, that consists of the heart and blood vessels. The circulatory system has two divisions, a systemic circulation or circuit, and a pulmonary circulation or circuit. Some sources use the terms cardiovascular system and vascular system interchangeably with circulatory system.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Cardiopulmonary Bypass (CPB) is a machine that temporarily takes over the function of the heart and lungs during a cardiac surgery by maintaining the circulation of blood and oxygen throughout the body.

Extracorporeal membrane oxygenation (ECMO), is a form of extracorporeal life support, providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
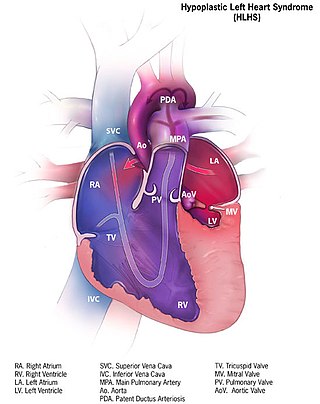
Hypoplastic left heart syndrome (HLHS) is a rare congenital heart defect in which the left side of the heart is severely underdeveloped and incapable of supporting the systemic circulation. It is estimated to account for 2-3% of all congenital heart disease. Early signs and symptoms include poor feeding, cyanosis, and diminished pulse in the extremities. The etiology is believed to be multifactorial resulting from a combination of genetic mutations and defects resulting in altered blood flow in the heart. Several structures can be affected including the left ventricle, aorta, aortic valve, or mitral valve all resulting in decreased systemic blood flow.

The cardiac cycle is the performance of the human heart from the beginning of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, following a period of robust contraction and pumping of blood, called systole. After emptying, the heart relaxes and expands to receive another influx of blood returning from the lungs and other systems of the body, before again contracting to pump blood to the lungs and those systems.
Pulsus paradoxus, also paradoxic pulse or paradoxical pulse, is an abnormally large decrease in stroke volume, systolic blood pressure and pulse wave amplitude during inspiration. Pulsus paradoxus is not related to pulse rate or heart rate, and it is not a paradoxical rise in systolic pressure. Normally, blood pressure drops less precipitously than 10 mmHg during inhalation. Pulsus paradoxus is a sign that is indicative of several conditions, most commonly pericardial effusion.

A ventricular assist device (VAD) is an electromechanical device that provides support for cardiac circulation, which is used either to partially or to completely replace the function of a failing heart. VADs can be used in patients with acute or chronic heart failure, which can occur due to a variety of reasons.
The intra-aortic balloon pump (IABP) is a mechanical device that increases myocardial oxygen perfusion and indirectly increases cardiac output through afterload reduction. It consists of a cylindrical polyurethane balloon that sits in the aorta, approximately 2 centimeters (0.79 in) from the left subclavian artery. The balloon inflates and deflates via counter pulsation, meaning it actively deflates in systole and inflates in diastole. Systolic deflation decreases afterload through a vacuum effect and indirectly increases forward flow from the heart. Diastolic inflation increases blood flow to the coronary arteries via retrograde flow. These actions combine to decrease myocardial oxygen demand and increase myocardial oxygen supply.
A right-to-left shunt is a cardiac shunt which allows blood to flow from the right heart to the left heart. This terminology is used both for the abnormal state in humans and for normal physiological shunts in reptiles.
Abiomed, Inc. is a medical device technology company that operates as a stand-alone business within Johnson & Johnson's MedTech Segment. Abiomed develops and manufactures temporary external and implantable mechanical circulatory support devices. The company is headquartered in Danvers, Massachusetts with additional offices in Woburn, Baltimore, Berlin, Aachen, and Tokyo.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.
The Hemopump was designed to allow for temporary support of a failing heart. It is a continuous flow pump, and does not need to be synced to the rhythm of the heart. It assists in temporary heart stimulation with conditions such as cardiogenic shock following acute myocardial infarction, heart failure from cardiopulmonary bypass, and more. The pump can continually monitor the left ventricle, which allows for perpetual observation of the hearts condition. This allows for any necessary changes to be made when needed. The pump operates at speeds between two hundred and ninety and four hundred and seventy revolutions per minute.
A plot of a system's pressure versus volume has long been used to measure the work done by the system and its efficiency. This analysis can be applied to heat engines and pumps, including the heart. A considerable amount of information on cardiac performance can be determined from the pressure vs. volume plot. A number of methods have been determined for measuring PV-loop values experimentally.
Impella is a family of medical devices used for temporary ventricular support in patients with depressed heart function. Some versions of the device can provide left heart support during other forms of mechanical circulatory support including ECMO and Centrimag.

Heart development, also known as cardiogenesis, refers to the prenatal development of the heart. This begins with the formation of two endocardial tubes which merge to form the tubular heart, also called the primitive heart tube. The heart is the first functional organ in vertebrate embryos.

Acute cardiac unloading is any maneuver, therapy, or intervention that decreases the power expenditure of the ventricle and limits the hemodynamic forces that lead to ventricular remodeling after insult or injury to the heart. This technique is being investigated as a therapeutic to aid after damage has occurred to the heart, such as after a heart attack. The theory behind this approach is that by simultaneously limiting the oxygen demand and maximizing oxygen delivery to the heart after damage has occurred, the heart is more fully able to recover. This is primarily achieved by using temporary minimally invasive mechanical circulatory support to supplant the pumping of blood by the heart. Using mechanical support decreases the workload of the heart, or unloads it.
The main pathophysiology of heart failure is a reduction in the efficiency of the heart muscle, through damage or overloading. As such, it can be caused by a wide number of conditions, including myocardial infarction, hypertension and cardiac amyloidosis. Over time these increases in workload will produce changes to the heart itself:
References
- 1 2 3 "UOTW #7 – Ultrasound of the Week". Ultrasound of the Week. 30 June 2014. Retrieved 27 May 2017.
- 1 2 3 "Cardiogenic shock – Symptoms and causes". Mayo Clinic. Retrieved 22 May 2020.
- ↑ Schrage B, Becher PM, Goßling A, Savarese G, Dabboura S, Yan I, et al. (April 2021). "Temporal trends in incidence, causes, use of mechanical circulatory support and mortality in cardiogenic shock". ESC Heart Failure. 8 (2): 1295–1303. doi:10.1002/ehf2.13202. PMC 8006704 . PMID 33605565.
- 1 2 3 4 5 6 Vahdatpour C, Collins D, Goldberg S (April 2019). "Cardiogenic Shock". Journal of the American Heart Association. 8 (8): e011991. doi:10.1161/JAHA.119.011991. PMC 6507212 . PMID 30947630.
- ↑ Thiele H, de Waha-Thiele S, Freund A, Zeymer U, Desch S, Fitzgerald S (August 2021). "Management of cardiogenic shock". EuroIntervention. 17 (6): 451–465. doi:10.4244/EIJ-D-20-01296. PMC 9724885 . PMID 34413010.
- ↑ International Trauma Life Support for Emergency Care Providers (8 ed.). Pearson Education Limited. 2018. pp. 172–173. ISBN 978-1292-17084-8.
- ↑ Rippe JM, Irwin RS (2003). Irwin and Rippe's intensive care medicine. Philadelphia: Lippincott Williams & Wilkins. ISBN 978-0-7817-3548-3. OCLC 53868338.[ page needed ]
- ↑ Marino PL (1998). The ICU book. Baltimore: Williams & Wilkins. ISBN 978-0-683-05565-8. OCLC 300112092.[ page needed ]
- ↑ Society of Critical Care Medicine. (2001). Fundamental Critical Care Support. Society of Critical Care Medicine. ISBN 978-0-936145-02-0. OCLC 48632566.[ page needed ]
- ↑ Harrison's Principles of Internal Medicine (16th ed.). The McGraw-Hill Companies. 2005. ISBN 0-07-140235-7. Archived from the original on 2012-08-04.
- ↑ Goldman L, Ausiello D, eds. (2003). Cecil Textbook of Medicine (22nd ed.). W. B. Saunders Company. ISBN 0-7216-9652-X. Archived from the original on 2010-06-16.
- ↑ Warrell DA, Cox TM, Firth JD, Benz EJ, eds. (2003). The Oxford Textbook of Medicine (Fourth ed.). Oxford University Press. ISBN 0-19-262922-0. Archived from the original on 2006-09-23.
- ↑ Cheatham ML, Block EF, Smith HG, Promes JT. Shock: An Overview (PDF). Surgical Critical Care Service, Department of Surgical Education (Report). Orlando, Florida: Orlando Regional Medical Center. Archived from the original (PDF) on 2017-06-22.
- ↑ "Cardiogenic shock". Department of Anaesthesia and Intensive Care of The Chinese University of Hong Kong . Archived from the original on 2017-07-23.
- ↑ "Introduction to management of shock for junior ICU trainees and medical students". Department of Anaesthesia and Intensive Care of The Chinese University of Hong Kong . Archived from the original on 2017-07-27.
- 1 2 3 Geller BJ, Sinha SS, Kapur NK, Bakitas M, Balsam LB, Chikwe J, et al. (August 2022). "Escalating and De-escalating Temporary Mechanical Circulatory Support in Cardiogenic Shock: A Scientific Statement From the American Heart Association". Circulation. 146 (6): e50–e68. doi: 10.1161/CIR.0000000000001076 . PMID 35862152.
- 1 2 3 4 5 6 7 Combes A, Price S, Slutsky AS, Brodie D (July 2020). "Temporary circulatory support for cardiogenic shock". Lancet. 396 (10245): 199–212. doi: 10.1016/S0140-6736(20)31047-3 . PMID 32682486.
- ↑ Ni Hlci, Tamara; Boardman, Henry MP; Baig, Kamran; Aifesehi, Paul E.; Stafford, Jody L.; Cernei, Cristina; Bodger, Owen; Westaby, Stephen; et al. (Cochrane Heart Group) (2018-04-12). "Mechanical assist devices for acute cardiogenic shock". Cochrane Database of Systematic Reviews. 2018 (4): CD013002. doi:10.1002/14651858.CD013002. PMC 6494568 .
- ↑ Russo JJ, Aleksova N, Pitcher I, Couture E, Parlow S, Faraz M, et al. (February 2019). "Left Ventricular Unloading During Extracorporeal Membrane Oxygenation in Patients With Cardiogenic Shock". Journal of the American College of Cardiology. 73 (6): 654–662. doi: 10.1016/j.jacc.2018.10.085 . PMID 30765031.