Diagnosis
| | This section is empty. You can help by adding to it. (February 2019) |
| Distributive shock |
|---|
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. [1] [2] It is one of four categories of shock, a condition where there is not enough oxygen-carrying blood to meet the metabolic needs of the cells which make up the body's tissues and organs. [2] Distributive shock is different from the other three categories of shock in that it occurs even though the output of the heart is at or above a normal level. [2] The most common cause is sepsis leading to a type of distributive shock called septic shock, a condition that can be fatal. [1]
Elbers and Ince have identified five classes of abnormal microcirculatory flow in distributive shock using side stream dark field microscopy.
According to the cause, there are 4 types of distributive shock:
In addition to sepsis, distributive shock can be caused by systemic inflammatory response syndrome (SIRS) due to conditions other than infection such as pancreatitis, burns or trauma. [3] Other causes include, toxic shock syndrome (TSS), anaphylaxis (a sudden, severe allergic reaction), adrenal insufficiency, reactions to drugs or toxins, heavy metal poisoning, hepatic (liver) insufficiency and damage to the central nervous system. [3] Causes of adrenal insufficiency leading to distributive shock include acute worsening of chronic adrenal insufficiency, destruction or removal of the adrenal glands, suppression of adrenal gland function due to exogenous steroids, hypopituitarism and metabolic failure of hormone production. [3]
The cause of inadequate tissue perfusion (blood delivery to tissues) in distributive shock is a lack of normal responsiveness of blood vessels to vasoconstrictive agents and direct vasodilation. [4]
There are four types of distributive shock. The most common, septic shock, is caused by an infection, most frequently by bacteria, but viruses, fungi and parasites have been implicated. [3] Infection sites most likely to lead to septic shock are chest, abdomen and genitourinary tract. [3] In septic shock the blood flow in the microvasculature is abnormal with some capillaries underperfused and others with normal to high blood flow. [5] The endothelial cells lining the blood vessels become less responsive to vasocontrictive agents, lose their glycocalyx (normal coating) and negative ionic charge, become leaky and cause extensive over-expression of nitric oxide. [2] The coagulation cascade is also disrupted. [4] Tissue factor that initiates the clotting cascade is produced by activated monocytes and the endothelial cells lining the blood vessels while antithrombin and fibrinolysis are impaired. [4] Disseminated intravascular coagulation (DIC) can result from the thrombin produced in the inflammatory response. [4] The ability of red blood cells to change shape decreases and their tendency to clump together increases, inhibiting their flow through the microvasculature. [5]
In anaphylactic shock low blood pressure is related to decreased systemic vascular resistance (SVR) triggered primarily by a massive release of histamine by mast cells activated by antigen-bound immunoglobulin E and also by increased production and release of prostaglandins. [4]
Neurogenic shock is caused by the loss of vascular tone normally supported by the sympathetic nervous system due to injury to the central nervous system especially spinal cord injury. [4] [6] Rupture of a hollow organ, with subsequent evacuation of contents in the peritoneal cavity could also determine neurogenic shock, a subtype of distributive shock. This happens due to the widespread peritoneal irritation by the ruptured viscus contents, as in peptic ulcer perforation, with consequent strong vagal activation, and generalized, extensive peripheral vasodilation and bradycardia. [7] [8] Thus, in neurogenic shock, there is decreased systemic vascular resistance, CVP is typically decreased, CO decreased or normal, and PAOP decreased. [2]
Distributive shock associated with adrenal crisis results from inadequate steroid hormones.
| | This section is empty. You can help by adding to it. (February 2019) |
The main goals of treatment in distributive shock are to reverse the underlying cause and achieve hemodynamic stabilization. [9] Immediate treatment involves fluid resuscitation and the use of vasoactive drugs, both vasopressors and inotropes. [10] Hydrocortisone is used for people whose hypotension does not respond to fluid resuscitation and vasopressors. [11] Opening and keeping open the microcirculation is a consideration in the treatment of distributive shock, as a result limiting the use of vasopressors has been suggested. [2] Control of inflammation, vascular function and coagulation to correct pathological differences in blood flow and microvascular shunting has been pointed to as a potentially important adjunct goal in the treatment of distributive shock. [2]
People with septic shock are treated with antimicrobial drugs to treat the causative infection. [12] Some sources of infection require surgical intervention including necrotizing fasciitis, cholangitis, abscess, intestinal ischemia, or infected medical devices. [13]
Anaphylactic shock is treated with epinephrine. [14] The use of vasopressin together with norepinephrine rather than norepinephrine alone appears to decrease the risk of atrial fibrillation but with few other benefits. [15]
Septic shock is associated with significant mortality and is the leading non-cardiac cause of death in intensive care units (ICUs). [1]
The choice of fluids for resuscitation remains an area of research, the Surviving Sepsis Campaign an international consortium of experts, did not find adequate evidence to support the superiority crystalloid fluids versus colloid fluids. [10] Drugs such as, pyridoxalated hemoglobin polyoxyethylene, which scavenge nitric oxide from the blood have been investigated. [16] As well as methylene blue which may inhibit the nitric oxide-cyclic guanosine monophosphate (NO-cGMP) pathway which has been suggested to play a significant role in distributive shock. [17]

Waterhouse–Friderichsen syndrome (WFS) is defined as adrenal gland failure due to bleeding into the adrenal glands, commonly caused by severe bacterial infection. Typically, it is caused by Neisseria meningitidis.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.

The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid and electrolyte balance, and systemic vascular resistance.

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.
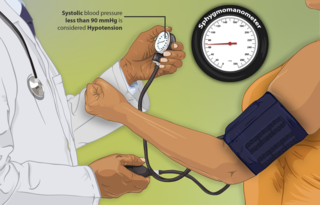
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
In immunology, systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, it actually has pro- and anti-inflammatory components.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

Neurogenic shock is a distributive type of shock resulting in hypotension, often with bradycardia, caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nervous system, such as spinal cord injury and traumatic brain injury. Low blood pressure occurs due to decreased systemic vascular resistance resulting from loss of sympathetic tone, which in turn causes blood pooling within the extremities rather than being available to circulate throughout the body. The slowed heart rate results from a vagal response unopposed by a sympathetic nervous system (SNS) response. Such cardiovascular instability is exacerbated by hypoxia, or treatment with endotracheal or endobronchial suction used to prevent pulmonary aspiration.
End organ damage is severe impairment of major body organs due to high blood pressure or states of low blood pressure or low blood volume. This can present as a heart attack or heart failure, pulmonary edema, neurologic deficits including a stroke, or acute kidney failure.
Capillary leak syndrome, or vascular leak syndrome, is characterized by the escape of blood plasma through capillary walls, from the blood circulatory system to surrounding tissues, muscle compartments, organs or body cavities. It is a phenomenon most commonly witnessed in sepsis, and less frequently in autoimmune diseases, differentiation syndrome, engraftment syndrome, hemophagocytic lymphohistiocytosis, the ovarian hyperstimulation syndrome, viral hemorrhagic fevers, and snakebite and ricin poisoning. Pharmaceuticals, including the chemotherapy medications gemcitabine and denileukin diftitox, as well as certain interleukins and monoclonal antibodies, can also cause capillary leaks. These conditions and factors are sources of secondary capillary leak syndrome.
The Surviving Sepsis Campaign (SSC) is a global initiative to bring together professional organizations in reducing mortality from sepsis. The purpose of the SSC is to create an international collaborative effort to improve the treatment of sepsis and reduce the high mortality rate associated with the condition. The Surviving Sepsis Campaign and the Institute for Healthcare Improvement have teamed up to achieve a 25 percent reduction in sepsis mortality by 2009. The guidelines were updated in 2016 and again in 2021.
Early goal-directed therapy was introduced by Emanuel P. Rivers in The New England Journal of Medicine in 2001 and is a technique used in critical care medicine involving intensive monitoring and aggressive management of perioperative hemodynamics in patients with a high risk of morbidity and mortality. In cardiac surgery, goal-directed therapy has proved effective when commenced after surgery. The combination of GDT and Point-of-Care Testing has demonstrated a marked decrease in mortality for patients undergoing congenital heart surgery. Furthermore, a reduction in morbidity and mortality has been associated with GDT techniques when used in conjunction with an electronic medical record.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.

Norepinephrine, also known as noradrenaline, is a medication used to treat people with very low blood pressure. It is the typical medication used in sepsis if low blood pressure does not improve following intravenous fluids. It is the same molecule as the hormone and neurotransmitter norepinephrine. It is given by slow injection into a vein.

Angiotensin II is a medication that is used to treat hypotension resulting from septic shock or other distributive shock. It is a synthetic vasoconstrictor peptide that is identical to human hormone angiotensin II and is marketed under the brand name Giapreza. The Food and Drug Administration approved the use of angiotensin II in December 2017 to treat low blood pressure resulting from septic shock.
Vasodilatory shock, vasogenic shock, or vasoplegic shock is a medical emergency belonging to shock along with cardiogenic shock, septic shock, allergen-induced shock and hypovolemic shock. When the blood vessels suddenly relax, it results in vasodilation. In vasodilatory shock, the blood vessels are too relaxed leading to extreme vasodilation and blood pressure drops and blood flow becomes very low. Without enough blood pressure, blood and oxygen will not be pushed to reach the body's organs. If vasodilatory shock lasts more than a few minutes, the lack of oxygen starts to damage the body's organs. Vasodilatory shock like other types of shock should be treated quickly, otherwise it can cause permanent organ damage or death as a result of multiple organ dysfunction.
{{cite journal}}: CS1 maint: multiple names: authors list (link)