Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Hemoglobinopathy is the medical term for a group of inherited blood disorders and diseases that primarily affect red blood cells. They are single-gene disorders and, in most cases, they are inherited as autosomal co-dominant traits.

Anemia or anaemia is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin or hemoglobin abnormalities. The name is derived from Ancient Greek: ἀναιμία anaimia, meaning 'lack of blood', from ἀν- an-, 'not' and αἷμα haima, 'blood'. When anemia comes on slowly, the symptoms are often vague, such as tiredness, weakness, shortness of breath, headaches, and a reduced ability to exercise. When anemia is acute, symptoms may include confusion, feeling like one is going to pass out, loss of consciousness, and increased thirst. Anemia must be significant before a person becomes noticeably pale. Symptoms of anemia depend on how quickly hemoglobin decreases. Additional symptoms may occur depending on the underlying cause. Preoperative anemia can increase the risk of needing a blood transfusion following surgery. Anemia can be temporary or long term and can range from mild to severe.
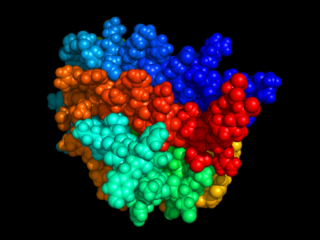
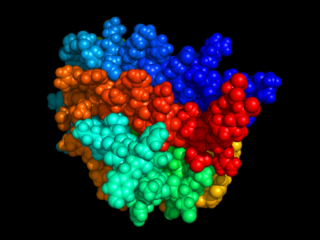
Erythropoietin, also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidneys in response to cellular hypoxia; it stimulates red blood cell production (erythropoiesis) in the bone marrow. Low levels of EPO are constantly secreted in sufficient quantities to compensate for normal red blood cell turnover. Common causes of cellular hypoxia resulting in elevated levels of EPO include any anemia, and hypoxemia due to chronic lung disease.
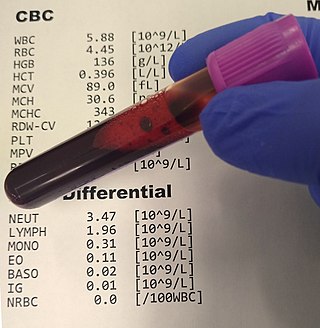
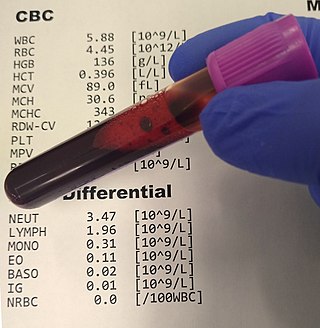
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and platelets, the concentration of hemoglobin, and the hematocrit. The red blood cell indices, which indicate the average size and hemoglobin content of red blood cells, are also reported, and a white blood cell differential, which counts the different types of white blood cells, may be included.

The hematocrit, also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is normally 40.7–50.3% for males and 36.1–44.3% for females. It is a part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count and platelet count.

In oncology, polycythemia vera is an uncommon myeloproliferative neoplasm in which the bone marrow makes too many red blood cells as well as white blood cells and platelets.

In hematology, essential thrombocythemia (ET) is a rare chronic blood cancer characterised by the overproduction of platelets (thrombocytes) by megakaryocytes in the bone marrow. It may, albeit rarely, develop into acute myeloid leukemia or myelofibrosis. It is one of the blood cancers wherein the bone marrow produces too many white or red blood cells, or platelets.

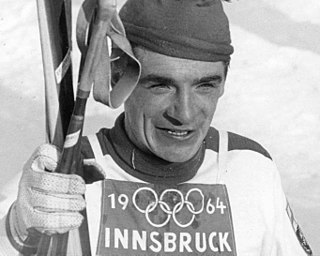
Altitude training is the practice by some endurance athletes of training for several weeks at high altitude, preferably over 2,400 metres (8,000 ft) above sea level, though more commonly at intermediate altitudes due to the shortage of suitable high-altitude locations. At intermediate altitudes, the air still contains approximately 20.9% oxygen, but the barometric pressure and thus the partial pressure of oxygen is reduced.
Primary myelofibrosis (PMF) is a rare bone marrow blood cancer. It is classified by the World Health Organization (WHO) as a type of myeloproliferative neoplasm, a group of cancers in which there is activation and growth of mutated cells in the bone marrow. This is most often associated with a somatic mutation in the JAK2, CALR, or MPL genes. In PMF, the bony aspects of bone marrow are remodeled in a process called osteosclerosis; in addition, fibroblast secrete collagen and reticulin proteins that are collectively referred to as (fibrosis). These two pathological processes compromise the normal function of bone marrow resulting in decreased production of blood cells such as erythrocytes, granulocytes and megakaryocytes, the latter cells responsible for the production of platelets.

Myeloproliferative neoplasms (MPNs) are a group of rare blood cancers in which excess red blood cells, white blood cells or platelets are produced in the bone marrow. Myelo refers to the bone marrow, proliferative describes the rapid growth of blood cells and neoplasm describes that growth as abnormal and uncontrolled.
Blood doping is a form of doping in which the number of red blood cells in the bloodstream is boosted in order to enhance athletic performance. Because such blood cells carry oxygen from the lungs to the muscles, a higher concentration in the blood can improve an athlete's aerobic capacity (VO2 max) and endurance. Blood doping can be achieved by making the body produce more red blood cells itself using drugs, giving blood transfusions either from another person or back to the same individual, or by using blood substitutes.
Anemia of chronic disease (ACD) or anemia of chronic inflammation is a form of anemia seen in chronic infection, chronic immune activation, and malignancy. These conditions all produce elevation of interleukin-6, which stimulates hepcidin production and release from the liver. Hepcidin production and release shuts down ferroportin, a protein that controls export of iron from the gut and from iron storing cells. As a consequence, circulating iron levels are reduced. Other mechanisms may also play a role, such as reduced erythropoiesis. It is also known as anemia of inflammation, or anemia of inflammatory response.
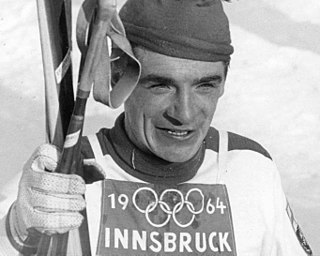
Eero Antero Mäntyranta was one of the most successful Finnish cross-country skiers. He competed in four Winter Olympics (1960–1972) winning seven medals at three of them. His performance at the 1964 Winter Olympics earned him the nickname "Mister Seefeld", referring to the venue where the cross-country skiing and biathlon competitions took place. The Finnish Ministry of Education endowed him with the Pro Urheilu letter of recognition in 2000. There is also a museum centered on Mäntyranta in his birthplace of Pello.

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.

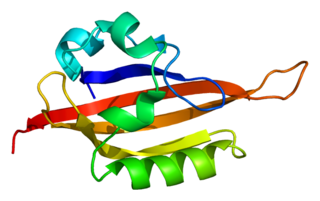
2,3-Bisphosphoglyceric acid (2,3-BPG), also known as 2,3-diphosphoglyceric acid (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyceric acid (1,3-BPG).
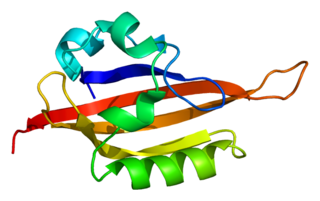
Endothelial PAS domain-containing protein 1 is a protein that is encoded by the EPAS1 gene in mammals. It is a type of hypoxia-inducible factor, a group of transcription factors involved in the physiological response to oxygen concentration. The gene is active under hypoxic conditions. It is also important in the development of the heart, and for maintaining the catecholamine balance required for protection of the heart. Mutation often leads to neuroendocrine tumors.

Basophilia is the condition of having greater than 200 basophils/μL in the venous blood. Basophils are the least numerous of the myelogenous cells, and it is rare for their numbers to be abnormally high without changes to other blood components. Rather, basophilia is most often coupled with other white blood cell conditions such as eosinophilia, high levels of eosinophils in the blood. Basophils are easily identifiable by a blue coloration of the granules within each cell, marking them as granulocytes, in addition to segmented nuclei.

Hemoglobinemia is a medical condition in which there is an excess of hemoglobin in the blood plasma. This is an effect of intravascular hemolysis, in which hemoglobin separates from red blood cells, a form of anemia.
Myomatous erythrocytosis syndrome(MES) is an uncommon gynecological disorder associated with isolated polycythemia and uterine fibroids. The primary feature of myomatous erythrocytosis syndrome is that hemoglobin goes back to its baseline level following the removal of the myoma. There have only been 50 cases of myomatous erythrocytosis syndrome documented as of 2023. Thomsen and Marson published the first case in 1953.