Constipation is a bowel dysfunction that makes bowel movements infrequent or hard to pass. The stool is often hard and dry. Other symptoms may include abdominal pain, bloating, and feeling as if one has not completely passed the bowel movement. Complications from constipation may include hemorrhoids, anal fissure or fecal impaction. The normal frequency of bowel movements in adults is between three per day and three per week. Babies often have three to four bowel movements per day while young children typically have two to three per day.

Fecal incontinence (FI), or in some forms, encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.
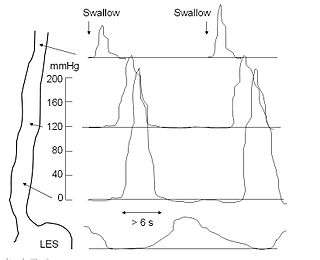
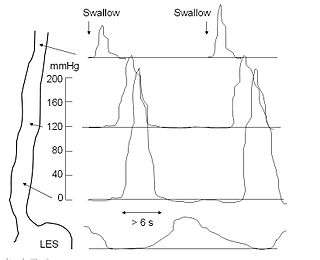
An esophageal motility study (EMS) or esophageal manometry is a test to assess motor function of the upper esophageal sphincter (UES), esophageal body and lower esophageal sphincter (LES).

An anal fissure is a break or tear in the skin of the anal canal. Anal fissures may be noticed by bright red anal bleeding on toilet paper and undergarments, or sometimes in the toilet. If acute they are painful after defecation, but with chronic fissures, pain intensity often reduces and becomes cyclical.

A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.

Colorectal surgery is a field in medicine dealing with disorders of the rectum, anus, and colon. The field is also known as proctology, but this term is now used infrequently within medicine and is most often employed to identify practices relating to the anus and rectum in particular. The word proctology is derived from the Greek words πρωκτός proktos, meaning "anus" or "hindparts", and -λογία -logia, meaning "science" or "study".
A fecal impaction or an impacted bowel is a solid, immobile bulk of feces that can develop in the rectum as a result of chronic constipation. Fecal impaction is a common result of neurogenic bowel dysfunction and causes immense discomfort and pain. Its treatment includes laxatives, enemas, and pulsed irrigation evacuation (PIE) as well as digital removal. It is not a condition that resolves without direct treatment.
The rectoanal inhibitory reflex (RAIR), also known as the anal sampling mechanism, anal sampling reflex, rectosphincteric reflex, or anorectal sampling reflex, is a reflex characterized by a transient involuntary relaxation of the internal anal sphincter in response to distention of the rectum. The RAIR provides the upper anal canal with the ability to discriminate between flatus and fecal material.

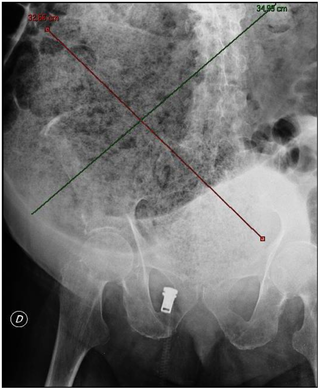
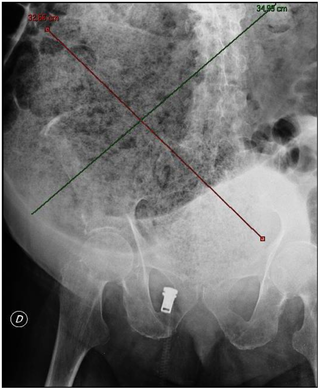
Defecography is a type of medical radiological imaging in which the mechanics of a patient's defecation are visualized in real time using a fluoroscope. The anatomy and function of the anorectum and pelvic floor can be dynamically studied at various stages during defecation.
Bowel management is the process which a person with a bowel disability uses to manage fecal incontinence or constipation. People who have a medical condition which impairs control of their defecation use bowel management techniques to choose a predictable time and place to evacuate. A simple bowel management technique might include diet control and establishing a toilet routine. As a more involved practice a person might use an enema to relieve themselves. Without bowel management, the person might either suffer from the feeling of not getting relief, or they might soil themselves.

The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about 12 centimetres (4.7 in) long, and begins at the rectosigmoid junction at the level of the third sacral vertebra or the sacral promontory depending upon what definition is used. Its diameter is similar to that of the sigmoid colon at its commencement, but it is dilated near its termination, forming the rectal ampulla. It terminates at the level of the anorectal ring or the dentate line, again depending upon which definition is used. In humans, the rectum is followed by the anal canal, which is about 4 centimetres (1.6 in) long, before the gastrointestinal tract terminates at the anal verge. The word rectum comes from the Latin rēctumintestīnum, meaning straight intestine.

In humans, the anus is the external opening of the rectum located inside the intergluteal cleft. Two sphincters control the exit of feces from the body during an act of defecation, which is the primary function of the anus. These are the internal anal sphincter and the external anal sphincter, which are circular muscles that normally maintain constriction of the orifice and which relax as required by normal physiological functioning. The inner sphincter is involuntary and the outer is voluntary. Above the anus is the perineum, which is also located beneath the vulva or scrotum.
Solitary rectal ulcer syndrome or SRUS is a chronic, benign disorder of the rectal mucosa. It commonly occurs with varying degrees of rectal prolapse. The condition is thought to be caused by different factors, such as long term constipation, straining during defecation, and dyssynergic defecation. Treatment is by normalization of bowel habits, biofeedback, and other conservative measures. In more severe cases various surgical procedures may be indicated. The condition is relatively rare, affecting approximately 1 in 100,000 people per year. It affects mainly adults aged 30–50. Females are affected slightly more often than males. The disorder can be confused clinically with rectal cancer or other conditions such as inflammatory bowel disease, even when a biopsy is done.

Anismus or dyssynergic defecation is the failure of normal relaxation of pelvic floor muscles during attempted defecation. It can occur in both children and adults, and in both men and women. It can be caused by physical defects or it can occur for other reasons or unknown reasons. Anismus that has a behavioral cause could be viewed as having similarities with parcopresis, or psychogenic fecal retention.
Obstructed defecation syndrome is a major cause of functional constipation, of which it is considered a subtype. It is characterized by difficult and/or incomplete emptying of the rectum with or without an actual reduction in the number of bowel movements per week. Normal definitions of functional constipation include infrequent bowel movements and hard stools. In contrast, ODS may occur with frequent bowel movements and even with soft stools, and the colonic transit time may be normal, but delayed in the rectum and sigmoid colon.
Dyssynergia is any disturbance of muscular coordination, resulting in uncoordinated and abrupt movements. This is also an aspect of ataxia. It is typical for dyssynergic patients to split a movement into several smaller movements. Types of dyssynergia include Ramsay Hunt syndrome type 1, bladder sphincter dyssynergia, and anal sphincter dyssynergia.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.

Neurogenic bowel dysfunction (NBD) is the inability to control defecation due to a deterioration of or injury to the nervous system, resulting in faecal incontinence or constipation. It is common in people with spinal cord injury (SCI), multiple sclerosis (MS) or spina bifida.

Satish Sanku Chander Rao is the J.Harold Harrison Distinguished University Chair in Gastroenterology at the Medical College of Georgia, Augusta University. He served as the former President of the American Neurogastroenterology and Motility Society and as Chair of the American Gastroenterological Association (AGA) Institute Council, Neurogastroenterology/Motility Section.
Low anterior resection syndrome is a complication of lower anterior resection, a type of surgery performed to remove the rectum, typically for rectal cancer. It is characterized by changes to bowel function that affect quality of life, and includes symptoms such as fecal incontinence, incomplete defecation or the sensation of incomplete defecation, changes in stool frequency or consistency, unpredictable bowel function, and painful defecation (dyschezia). Treatment options include symptom management, such as use of enemas, or surgical management, such as creation of a colostomy.