The term abdominal surgery broadly covers surgical procedures that involve opening the abdomen (laparotomy). Surgery of each abdominal organ is dealt with separately in connection with the description of that organ Diseases affecting the abdominal cavity are dealt with generally under their own names.
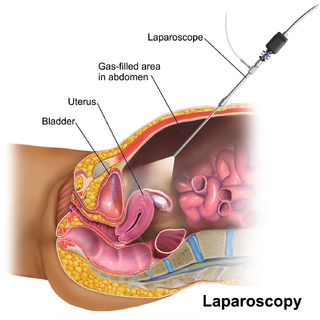
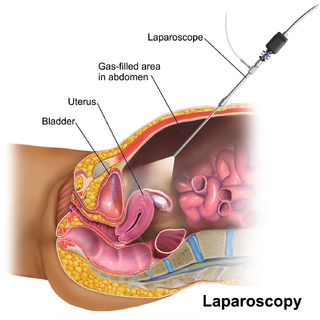
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.

Tubal ligation is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the implantation of a fertilized egg. Tubal ligation is considered a permanent method of sterilization and birth control.

Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.
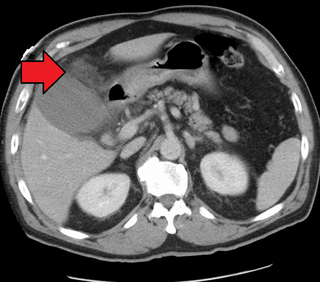
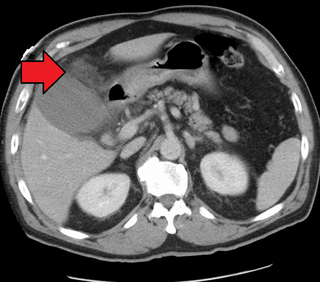
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks precede acute cholecystitis. The pain lasts longer in cholecystitis than in a typical gallbladder attack. Without appropriate treatment, recurrent episodes of cholecystitis are common. Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.
A laparotomy is a surgical procedure involving a surgical incision through the abdominal wall to gain access into the abdominal cavity. It is also known as a celiotomy.

Hysterectomy is the partial or total surgical removal of the uterus. It may also involve removal of the cervix, ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. Partial hysterectomies allow for hormone regulation while total hysterectomies do not.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

Diverticulitis, also called colonic diverticulitis, is a gastrointestinal disease characterized by inflammation of abnormal pouches—diverticula—that can develop in the wall of the large intestine. Symptoms typically include lower-abdominal pain of sudden onset, but the onset may also occur over a few days. There may also be nausea; and diarrhea or constipation. Fever or blood in the stool suggests a complication. Repeated attacks may occur.

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.
An incisional hernia is a type of hernia caused by an incompletely-healed surgical wound. Since median incisions in the abdomen are frequent for abdominal exploratory surgery, ventral incisional hernias are often also classified as ventral hernias due to their location. Not all ventral hernias are from incisions, as some may be caused by other trauma or congenital problems.

Camran Nezhat, FACOG, FACS is an American laparoscopic surgeon, reproductive endocrinology and infertility sub-specialist who has been teaching and practicing medicine and surgery as an adjunct clinical professor of surgery, and obstetrics and gynecology at Stanford University Medical Center in Palo Alto, California since 1993. Nezhat is also chair of the Association of the Adjunct Clinical Faculty, Stanford University School of Medicine, and a clinical professor of OB/GYN at the University of California, San Francisco.
Tubal reversal, also called tubal sterilization reversal, tubal ligation reversal, or microsurgical tubal reanastomosis, is a surgical procedure that can restore fertility to women after a tubal ligation. By rejoining the separated segments of the fallopian tube, tubal reversal can give women the chance to become pregnant again. In some cases, however, the separated segments cannot actually be reattached to each other. In some cases the remaining segment of tube needs to be re-implanted into the uterus. In other cases, when the end of the tube has been removed, a procedure called a neofimbrioplasty must be performed to recreate a functional end of the tube which can then act like the missing fimbria and retrieve the egg that has been released during ovulation.

Fallopian tube obstruction, also known as fallopian tube occlusion is a major cause of female infertility. Blocked fallopian tubes are unable to let the ovum and the sperm converge, thus making fertilization impossible. Fallopian tubes are also known as oviducts, uterine tubes, and salpinges.
Pyloromyotomy is a surgical procedure in which a portion of the muscle fibers of the pyloric muscle are cut. This is typically done in cases where the contents from the stomach are inappropriately stopped by the pyloric muscle, causing the stomach contents to build up in the stomach and unable to be appropriately digested. The procedure is typically performed in cases of "hypertrophic pyloric stenosis" in young children. In most cases, the procedure can be performed with either an open approach or a laparoscopic approach and the patients typically have good outcomes with minimal complications.
Single-port laparoscopy (SPL) is a recently developed technique in laparoscopic surgery. It is a minimally invasive surgical procedure in which the surgeon operates almost exclusively through a single entry point, typically the patient's navel. Unlike a traditional multi-port laparoscopic approach, SPL leaves only a single small scar.
Single-incision laparoscopic surgery (SILS) is an advanced, minimally invasive (keyhole) procedure in which the surgeon operates almost exclusively through a single entry point, typically the patient's umbilicus (navel). Special articulating instruments and access ports eliminate the need to place trochars externally for triangulation, thus allowing the creation of a small, solitary portal of entry into the abdomen.
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) is a 501c6 non-profit professional organization providing education on gastrointestinal minimally invasive surgery. It describes itself thus: The mission of the Society of American Gastrointestinal and Endoscopic Surgeons is to innovate, educate and collaborate to improve patient care.

Kurt Karl Stephan Semm was a German gynecologist and pioneer in minimally invasive surgery. He has been called "the father of modern laparoscopy".
Henk de Kok was a Dutch surgeon born in 1931. While working at the Beatrix Hospital in Gorinchem, the Netherlands, he pioneered surgical laparoscopy and was the first worldwide to perform an appendectomy assisted by laparoscopy in 1975. Henk died 25 December 2020.