



Medical imaging in pregnancy may be indicated because of pregnancy complications, intercurrent diseases or routine prenatal care.




Medical imaging in pregnancy may be indicated because of pregnancy complications, intercurrent diseases or routine prenatal care.
Options for medical imaging in pregnancy include the following:

Magnetic resonance imaging (MRI), without MRI contrast agents, is not associated with any risk for the mother or the fetus, and together with medical ultrasonography, it is the technique of choice for medical imaging in pregnancy. [1]
For the first trimester, no known literature has documented specific adverse effects in human embryos or fetuses exposed to non-contrast MRI during the first trimester. [3] During the second and third trimesters, there is some evidence to support the absence of risk, including a retrospective study of 1737 prenatally exposed children, showing no significant difference in hearing, motor skills, or functional measures after a mean follow-up time of 2 years. [3]
Gadolinium contrast agents in the first trimester are associated with a slightly increased risk of a childhood diagnosis of several forms of rheumatism, inflammatory disorders, or infiltrative skin conditions, according to a retrospective study including 397 infants prenatally exposed to gadolinium contrast. [3] In the second and third trimesters, gadolinium contrast is associated with a slightly increased risk of stillbirth or neonatal death, by the same study. [3] Hence, is recommended that gadolinium contrast in MRI should be limited, and should only be used when it significantly improves diagnostic performance and is expected to improve fetal or maternal outcomes. [1]
Women have a legal right to not be forced to undergo medical imaging without first providing informed consent; a radiologist is usually the healthcare provider trained to enable informed consent. [4]
MRI is commonly used in pregnant women with acute abdominal pain and/or pelvic pain, or in suspected neurological disorders, placental diseases, tumors, infections, and/or cardiovascular diseases. [3] Appropriate use criteria by the American College of Radiology give a rating of ≥7 (usually appropriate) for non-contrast MRI for the following conditions:
Health effects of radiation may be grouped in two general categories:
The determinstistic effects have been studied at for example survivors of the atomic bombings of Hiroshima and Nagasaki and cases of where radiation therapy has been necessary during pregnancy:
| Gestational age | Embryonic age | Effects | Estimated threshold dose (mGy) |
|---|---|---|---|
| 2 to 4 weeks | 0 to 2 weeks | Miscarriage or none (all or nothing) | 50 - 100 [1] |
| 4 to 10 weeks | 2 to 8 weeks | Structural birth defects | 200 [1] |
| Growth restriction | 200 - 250 [1] | ||
| 10 to 17 weeks | 8 to 15 weeks | Severe intellectual disability | 60 - 310 [1] |
| 18 to 27 weeks | 16 to 25 weeks | Severe intellectual disability (lower risk) | 250 - 280 [1] |
The intellectual deficit has been estimated to be about 25 IQ-points per 1,000 mGy at 10 to 17 weeks of gestational age. [1]
| Imaging method | Fetal absorbed dose of ionizing radiation (mGy) |
|---|---|
| Projectional radiography | |
| Cervical spine by 2 views (anteroposterior and lateral) | < 0.001 [1] |
| Extremities | < 0.001 [1] |
| Mammography by 2 views | 0.001 - 0.01 [1] |
| Chest | 0.0005 - 0.01 [1] |
| Abdominal | 0.1 - 3.0 [1] |
| Lumbar spine | 1.0 - 10 [1] |
| Intravenous pyelogram | 5 - 10 [1] |
| Double contrast barium enema | 1.0 - 20 [1] |
| CT scan | |
| Head or neck | 1.0 - 10 [1] |
| Chest, including CT pulmonary angiogram | 0.01 - 0.66 [1] |
| Limited CT pelvimetry by single axial slice through femoral heads | < 1 [1] |
| Abdominal | 1.3 - 35 [1] |
| Pelvic | 10 - 50 [1] |
| Nuclear medicine | |
| Low-dose perfusion scintigraphy | 0.1 - 0.5 [1] |
| Bone scintigraphy with 99mTc | 4 - 5 [1] |
| Pulmonary digital subtraction angiography | 0.5 [1] |
| Whole-body PET/CT with 18F' | 10 - 15 [1] |
The risk for the mother of later acquiring radiation-induced breast cancer seems to be particularly high for radiation doses during pregnancy. [6]
This is an important factor when for example determining whether a ventilation/perfusion scan (V/Q scan) or a CT pulmonary angiogram (CTPA) is the optimal investigation in pregnant women with suspected pulmonary embolism. A V/Q scan confers a higher radiation dose to the fetus, while a CTPA confers a much higher radiation dose to the mother's breasts. A review from the United Kingdom in 2005 considered CTPA to be generally preferable in suspected pulmonary embolism in pregnancy because of higher sensitivity and specificity as well as a relatively modest cost. [7]

A computed tomography scan is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or radiology technologists.
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgical field.

Medical ultrasound includes diagnostic techniques using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, muscles, joints, blood vessels, and internal organs, to measure some characteristics or to generate an informative audible sound. The usage of ultrasound to produce visual images for medicine is called medical ultrasonography or simply sonography, or echography. The practice of examining pregnant women using ultrasound is called obstetric ultrasonography, and was an early development of clinical ultrasonography. The machine used is called an ultrasound machine, a sonograph or an echograph. The visual image formed using this technique is called an ultrasonogram, a sonogram or an echogram.

Radiology is the medical discipline that uses medical imaging to diagnose diseases and guide their treatment, within the bodies of humans and other animals. It began with radiography, but today it includes all imaging modalities, including those that use no electromagnetic radiation, as well as others that do, such as computed tomography (CT), fluoroscopy, and nuclear medicine including positron emission tomography (PET). Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Obstetric ultrasonography, or prenatal ultrasound, is the use of medical ultrasonography in pregnancy, in which sound waves are used to create real-time visual images of the developing embryo or fetus in the uterus (womb). The procedure is a standard part of prenatal care in many countries, as it can provide a variety of information about the health of the mother, the timing and progress of the pregnancy, and the health and development of the embryo or fetus.

Prenatal testing is a tool that can be used to detect some birth defects at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, trisomy 18, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.
Radiocontrast agents are substances used to enhance the visibility of internal structures in X-ray-based imaging techniques such as computed tomography, projectional radiography, and fluoroscopy. Radiocontrast agents are typically iodine, or more rarely barium sulfate. The contrast agents absorb external X-rays, resulting in decreased exposure on the X-ray detector. This is different from radiopharmaceuticals used in nuclear medicine which emit radiation.
Prenatal development includes the development of the embryo and of the fetus during a viviparous animal's gestation. Prenatal development starts with fertilization, in the germinal stage of embryonic development, and continues in fetal development until birth.

Computed tomography angiography is a computed tomography technique used for angiography—the visualization of arteries and veins—throughout the human body. Using contrast injected into the blood vessels, images are created to look for blockages, aneurysms, dissections, and stenosis. CTA can be used to visualize the vessels of the heart, the aorta and other large blood vessels, the lungs, the kidneys, the head and neck, and the arms and legs. CTA can also be used to localise arterial or venous bleed of the gastrointestinal system.

A CT pulmonary angiogram (CTPA) is a medical diagnostic test that employs computed tomography (CT) angiography to obtain an image of the pulmonary arteries. Its main use is to diagnose pulmonary embolism (PE). It is a preferred choice of imaging in the diagnosis of PE due to its minimally invasive nature for the patient, whose only requirement for the scan is an intravenous line.
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI). The most commonly used compounds for contrast enhancement are gadolinium-based contrast agents (GBCAs). Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.

Gadobutrol (INN) (Gd-DO3A-butrol) is a gadolinium-based MRI contrast agent (GBCA).
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.
Prenatal memory, also called fetal memory, is important for the development of memory in humans. Many factors can impair fetal memory and its functions, primarily maternal actions. There are multiple techniques available not only to demonstrate the existence of fetal memory but to measure it. Fetal memory is vulnerable to certain diseases so much so that exposure can permanently damage the development of the fetus and even terminate the pregnancy by aborting the fetus. Maternal nutrition and the avoidance of drugs, alcohol and other substances during all nine months of pregnancy is important to the development of the fetus and its memory systems. The use of certain substances can entail long-term permanent effects on the fetus that can carry on throughout their lifespan.

Contrast CT, or contrast enhanced computed tomography (CECT), is X-ray computed tomography (CT) using radiocontrast. Radiocontrasts for X-ray CT are generally iodine-based types. This is useful to highlight structures such as blood vessels that otherwise would be difficult to delineate from their surroundings. Using contrast material can also help to obtain functional information about tissues. Often, images are taken both with and without radiocontrast. CT images are called precontrast or native-phase images before any radiocontrast has been administered, and postcontrast after radiocontrast administration.

Developmental toxicity is any developmental malformation that is caused by the toxicity of a chemical or pathogen. It is the structural or functional alteration, reversible or irreversible, which interferes with homeostasis, normal growth, differentiation, development or behavior. Developmental toxicity is caused by environmental insult, which includes drugs, alcohol, diet, toxic chemicals, and physical factors.
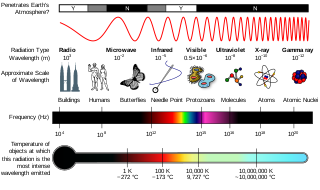
Radiation exposure is a measure of the ionization of air due to ionizing radiation from photons. It is defined as the electric charge freed by such radiation in a specified volume of air divided by the mass of that air. As of 2007, "medical radiation exposure" was defined by the International Commission on Radiological Protection as exposure incurred by people as part of their own medical or dental diagnosis or treatment; by persons, other than those occupationally exposed, knowingly, while voluntarily helping in the support and comfort of patients; and by volunteers in a programme of biomedical research involving their exposure. Common medical tests and treatments involving radiation include X-rays, CT scans, mammography, lung ventilation and perfusion scans, bone scans, cardiac perfusion scan, angiography, radiation therapy, and more. Each type of test carries its own amount of radiation exposure. There are two general categories of adverse health effects caused by radiation exposure: deterministic effects and stochastic effects. Deterministic effects are due to the killing/malfunction of cells following high doses; and stochastic effects involve either cancer development in exposed individuals caused by mutation of somatic cells, or heritable disease in their offspring from mutation of reproductive (germ) cells.

Magnetic resonance imaging (MRI) is in general a safe technique, although injuries may occur as a result of failed safety procedures or human error. During the last 150 years, thousands of papers focusing on the effects or side effects of magnetic or radiofrequency fields have been published. They can be categorized as incidental and physiological. Contraindications to MRI include most cochlear implants and cardiac pacemakers, shrapnel and metallic foreign bodies in the eyes. The safety of MRI during the first trimester of pregnancy is uncertain, but it may be preferable to other options. Since MRI does not use any ionizing radiation, its use generally is favored in preference to CT when either modality could yield the same information.