Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

Human chorionic gonadotropin (hCG) is a hormone for the maternal recognition of pregnancy produced by trophoblast cells that are surrounding a growing embryo, which eventually forms the placenta after implantation. The presence of hCG is detected in some pregnancy tests. Some cancerous tumors produce this hormone; therefore, elevated levels measured when the patient is not pregnant may lead to a cancer diagnosis and, if high enough, paraneoplastic syndromes, however, it is not known whether this production is a contributing cause, or an effect of carcinogenesis. The pituitary analog of hCG, known as luteinizing hormone (LH), is produced in the pituitary gland of males and females of all ages.

The chorion is the outermost fetal membrane around the embryo in mammals, birds and reptiles (amniotes). It develops from an outer fold on the surface of the yolk sac, which lies outside the zona pellucida, known as the vitelline membrane in other animals. In insects, it is developed by the follicle cells while the egg is in the ovary. Some mollusks also have chorions as part of their eggs. For example, fragile octopus eggs have only a chorion as their envelope.

The blastocyst is a structure formed in the early embryonic development of mammals. It possesses an inner cell mass (ICM) also known as the embryoblast which subsequently forms the embryo, and an outer layer of trophoblast cells called the trophectoderm. This layer surrounds the inner cell mass and a fluid-filled cavity known as the blastocoel. In the late blastocyst, the trophectoderm is known as the trophoblast. The trophoblast gives rise to the chorion and amnion, the two fetal membranes that surround the embryo. The placenta derives from the embryonic chorion and the underlying uterine tissue of the mother.

The female reproductive system is made up of the internal and external sex organs that function in the reproduction of new offspring. The human female reproductive system is immature at birth and develops to maturity at puberty to be able to produce gametes, and to carry a fetus to full term. The internal sex organs are the vagina, uterus, fallopian tubes, and ovaries. The female reproductive tract includes the vagina, uterus, and fallopian tubes and is prone to infections. The vagina allows for sexual intercourse and childbirth, and is connected to the uterus at the cervix. The uterus or womb accommodates the embryo, which develops into the fetus. The uterus also produces secretions, which help the transit of sperm to the fallopian tubes, where sperm fertilize ova produced by the ovaries. The external sex organs are also known as the genitals and these are the organs of the vulva including the labia, clitoris, and vaginal opening.

The trophoblast is the outer layer of cells of the blastocyst. Trophoblasts are present four days after fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures that do not directly contribute to the embryo. After blastulation, the trophoblast is contiguous with the ectoderm of the embryo and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency because they can no longer form a trophoblast. They become pluripotent stem cells.

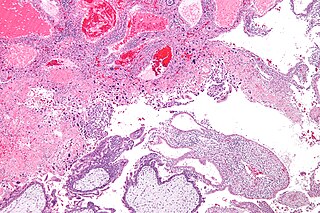
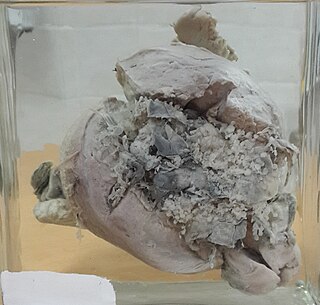
Choriocarcinoma is a malignant, trophoblastic cancer, usually of the placenta. It is characterized by early hematogenous spread to the lungs. It belongs to the malignant end of the spectrum in gestational trophoblastic disease (GTD). It is also classified as a germ cell tumor and may arise in the testis or ovary.
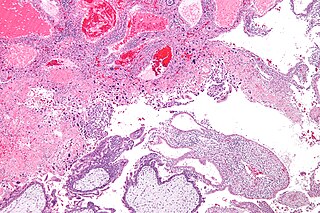
Gestational trophoblastic disease (GTD) is a term used for a group of pregnancy-related tumours. These tumours are rare, and they appear when cells in the womb start to proliferate uncontrollably. The cells that form gestational trophoblastic tumours are called trophoblasts and come from tissue that grows to form the placenta during pregnancy.
Gestational choriocarcinoma is a form of gestational trophoblastic neoplasia, which is a type of gestational trophoblastic disease (GTD), that can occur during pregnancy. It is a rare disease where the trophoblast, a layer of cells surrounding the blastocyst, undergoes abnormal developments, leading to trophoblastic tumors. The choriocarcinoma can metastasize to other organs, including the lungs, kidney, and liver. The amount and degree of choriocarcinoma spread to other parts of the body can vary greatly from person to person.

The human reproductive system includes the male reproductive system which functions to produce and deposit sperm; and the female reproductive system which functions to produce egg cells, and to protect and nourish the fetus until birth. Humans have a high level of sexual differentiation. In addition to differences in nearly every reproductive organ, there are numerous differences in typical secondary sex characteristics.
Dilation and evacuation (D&E) or dilatation and evacuation is the dilation of the cervix and surgical evacuation of the uterus after the first trimester of pregnancy. It is a method of abortion as well as a common procedure used after miscarriage to remove all pregnancy tissue.
Prenatal development includes the development of the embryo and of the fetus during a viviparous animal's gestation. Prenatal development starts with fertilization, in the germinal stage of embryonic development, and continues in fetal development until birth.
Gestational trophoblastic neoplasia (GTN) is group of rare diseases related to pregnancy and included in gestational trophoblastic disease (GTD) in which abnormal trophoblast cells grow in the uterus. GTN can be classified into benign and malignant lesions. Benign lesions include placental site nodule and hydatidiform moles while malignant lesions have four subtypes including invasive mole, gestational choriocarcinoma, placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT). The choriocarcinoma has 2 significant subtypes including gestational and non-gestational and they are differentiated by their different biological feature and prognosis. Signs and symptoms of GTN will appear vary from person to person and depending upon the type of the disease. They may include uterine bleeding not related to menstruation, pain or pressure in pelvis, large uterus and high blood pressure during pregnancy. The cause of this disease is unknown but the identification of the tumor based on total beta-human chorionic gonadotropin (β-hCG) in the serum.
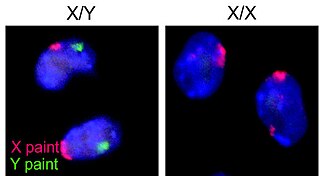
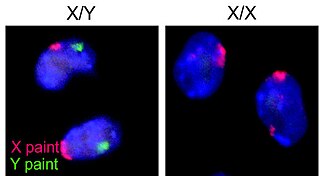
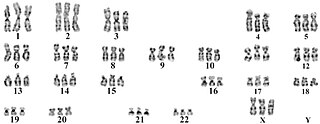
Human reproduction is sexual reproduction that results in human fertilization to produce a human offspring. It typically involves sexual intercourse between a sexually mature human male and female. During sexual intercourse, the interaction between the male and female reproductive systems results in fertilization of the ovum by the sperm to form a zygote. While normal cells contain 46 chromosomes, gamete cells only contain 23 single chromosomes, and it is when these two cells merge into one zygote cell that genetic recombination occurs and the new zygote contains 23 chromosomes from each parent, giving it 46 chromosomes. The zygote then undergoes a defined development process that is known as human embryogenesis, and this starts the typical 9-month gestation period that is followed by childbirth. The fertilization of the ovum may be achieved by artificial insemination methods, which do not involve sexual intercourse. Assisted reproductive technology also exists.

"Cytotrophoblast" is the name given to both the inner layer of the trophoblast or the cells that live there. It is interior to the syncytiotrophoblast and external to the wall of the blastocyst in a developing embryo.
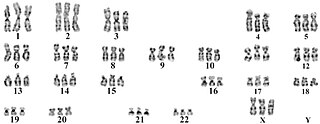
Triploid syndrome, also called triploidy, is a chromosomal disorder in which a fetus has three copies of every chromosome instead of the normal two. If this occurs in only some cells, it is called mosaic triploidy and is less severe.
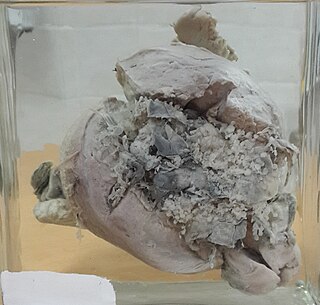
Invasive hydatidiform mole is a type of neoplasia that grows into the muscular wall of the uterus. It is formed after conception. It may spread to other parts of the body, such as the vagina, vulva, and lung.

A placental disease is any disease, disorder, or pathology of the placenta.

Placental site trophoblastic tumor is a form of gestational trophoblastic disease, which is thought to arise from intermediate trophoblast.
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.