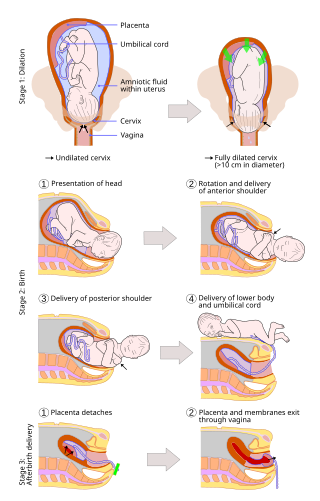
Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

Misoprostol is a synthetic prostaglandin medication used to prevent and treat stomach and duodenal ulcers, induce labor, cause an abortion, and treat postpartum bleeding due to poor contraction of the uterus. It is taken by mouth when used to prevent gastric ulcers in people taking nonsteroidal anti-inflammatory drugs (NSAID). For abortions it is used by itself or in conjunction with mifepristone or methotrexate. By itself, effectiveness for abortion is between 66% and 90%. For labor induction or abortion, it is taken by mouth, dissolved in the mouth, or placed in the vagina. For postpartum bleeding it may also be used rectally.
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing (starting) labor can be accomplished with pharmaceutical or non-pharmaceutical methods. In Western countries, it is estimated that one-quarter of pregnant women have their labor medically induced with drug treatment. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.
Rupture of membranes (ROM) or amniorrhexis is a term used during pregnancy to describe a rupture of the amniotic sac. Normally, it occurs spontaneously at full term either during or at the beginning of labor. Rupture of the membranes is known colloquially as "breaking (one's) water," especially when induced rather than spontaneous, or as one's "water breaking". A premature rupture of membranes (PROM) is a rupture of the amnion that occurs at full term and prior to the onset of labor. In cases of PROM, options include expectant management without intervention, or interventions such as oxytocin or other methods of labor induction, and both are usually accompanied by close monitoring of maternal and fetal health. Preterm premature rupture of membranes (PPROM) is when water breaks both before the onset of labor and before the pregnancy's 37 week gestation. In the United States, more than 120,000 pregnancies per year are affected by a premature rupture of membranes, which is the cause of about one third of preterm deliveries.
Bishop score, also Bishop's score or cervix score, is a pre-labor scoring system to assist in predicting whether induction of labor will be required. It has also been used to assess the likelihood of spontaneous preterm delivery. The Bishop score was developed by Professor Emeritus of Obstetrics and Gynecology, Edward Bishop, and was first published in August 1964.
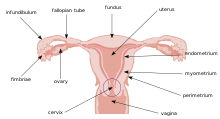
Cervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery. Cervical dilation may occur naturally, or may be induced surgically or medically.
Bloody show or show is the passage of a small amount of blood or blood-tinged mucus through the vagina near the end of pregnancy. It is caused by thinning and dilation of the cervix, leading to detachment of the cervical mucus plug that seals the cervix during pregnancy and tearing of small cervical blood vessels, and is one of the signs that labor may be imminent. The bloody show may be expelled from the vagina in pieces or altogether and often appears as a jelly-like piece of mucus stained with blood. Although the bloody show may be alarming at first, it is not a concern of patient health after 37 weeks gestation.
Fetal fibronectin (fFN) is a fibronectin protein produced by fetal cells. It is found at the interface of the chorion and the decidua. Fetal fibronectin is found normally in vaginal fluid in early pregnancy prior to 22 weeks due to normal growth and development of tissues at the junction of the uterus and amniotic sac. It may also be found in vaginal fluid after 36 weeks as labor approaches. However, fFN should not be detected between 22 and 36 weeks.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.
Cervical weakness, also called cervical incompetence or cervical insufficiency, is a medical condition of pregnancy in which the cervix begins to dilate (widen) and efface (thin) before the pregnancy has reached term. Definitions of cervical weakness vary, but one that is frequently used is the inability of the uterine cervix to retain a pregnancy in the absence of the signs and symptoms of clinical contractions, or labor, or both in the second trimester. Cervical weakness may cause miscarriage or preterm birth during the second and third trimesters. It has been estimated that cervical insufficiency complicates about 1% of pregnancies, and that it is a cause in about 8% of women with second trimester recurrent miscarriages.

Prostaglandin E2 (PGE2), also known as dinoprostone, is a naturally occurring prostaglandin with oxytocic properties that is used as a medication. Dinoprostone is used in labor induction, bleeding after delivery, termination of pregnancy, and in newborn babies to keep the ductus arteriosus open. In babies it is used in those with congenital heart defects until surgery can be carried out. It is also used to manage gestational trophoblastic disease. It may be used within the vagina or by injection into a vein.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.
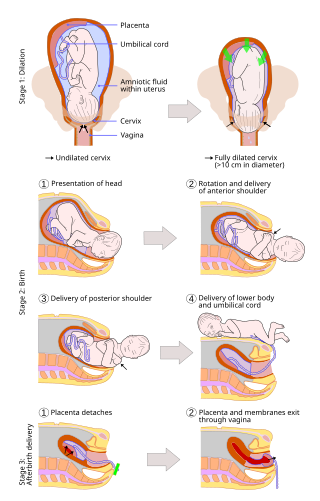
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than caesarean sections (C-sections).

Osmotic dilators are medical implements used to dilate the uterine cervix by swelling as they absorb fluid from surrounding tissue. They may be composed of natural or synthetic materials. A laminaria stick or tent is a thin rod made of the stems of dried Laminaria, a genus of kelp. Laminaria sticks can be generated from Laminaria japonica and Laminaria digitata. Synthetic osmotic dilators are commonly referred to by their brand names, such as Dilapan. Dilapan-S are composed of polyacrylonitrile, a plastic polymer. The hygroscopic nature of the polymer causes the dilator to absorb fluid and expand.
A uterotonic, also known as an oxytocic or ecbolic, is a type of medication used to induce contraction or greater tonicity of the uterus. Uterotonics are used both to induce labor and to reduce postpartum hemorrhage.
Artificial rupture of membranes (AROM), also known as an amniotomy, is performed by a midwife or obstetrician and was once thought to be an effective means to induce or accelerate labor. The membranes can be ruptured using a specialized tool, such as an amnihook or amnicot, or they may be ruptured by the proceduralist's finger. The different techniques for artificial rupture of membranes have not been extensively compared in the literature. In one study comparing amnihook versus amnicot for artificial rupture of membranes, use of an amnicot was associated with fewer neonatal scalp lacerations.
Uterine Tachysystole is a condition of excessively frequent uterine contractions during pregnancy. It is most often seen in induced or augmented labor, though it can also occur during spontaneous labor, and this may result in fetal hypoxia and acidosis. This may have serious effects on both the mother and the fetus including hemorrhaging and death. There are still major gaps in understanding treatment as well as clinical outcomes of this condition. Uterine tachysystole is defined as more than 5 contractions in 10 minutes, averaged over a 30-minute period.

Prolonged labor is the inability of a woman to proceed with childbirth upon going into labor. Prolonged labor typically lasts over 20 hours for first time mothers, and over 14 hours for women that have already had children. Failure to progress can take place during two different phases; the latent phase and active phase of labor. The latent phase of labor can be emotionally tiring and cause fatigue, but it typically does not result in further problems. The active phase of labor, on the other hand, if prolonged, can result in long term complications.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.