Midwifery is the health science and health profession that deals with pregnancy, childbirth, and the postpartum period, in addition to the sexual and reproductive health of women throughout their lives. In many countries, midwifery is a medical profession. A professional in midwifery is known as a midwife.

Caesarean section, also known as C-section or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen, often performed because vaginal delivery would put the baby or mother at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

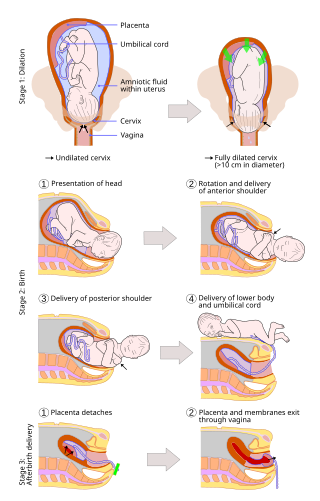
Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

Postpartum depression (PPD), also called postnatal depression, is a type of mood disorder experienced after childbirth, which can affect both sexes. Symptoms may include extreme sadness, low energy, anxiety, crying episodes, irritability, and changes in sleeping or eating patterns. PPD can also negatively affect the newborn child.

The postpartum period begins after childbirth and is typically considered to last for six weeks. However, there are three distinct but continuous phases of the postnatal period; the acute phase, lasting for six to twelve hours after birth; the subacute phase, lasting six weeks; and the delayed phase, lasting up to six months. During the delayed phase, some changes to the genitourinary system take much longer to resolve and may result in conditions such as urinary incontinence. The World Health Organization (WHO) describes the postnatal period as the most critical and yet the most neglected phase in the lives of mothers and babies; most maternal and newborn deaths occur during this period.

A maternal bond is the relationship between a mother and her child. While typically associated with pregnancy and childbirth, a maternal bond may also develop in cases where the child is unrelated, such as an adoption.

Placentophagy, also known as placentophagia, is the act of consuming part or all of the afterbirth following parturition in mammals. Parturition involves the delivery of the neonate, as well as the placenta and fetal membranes. The placenta is a critical organ that develops in the maternal uterus during pregnancy to support the fetus. It connects to the fetus via the umbilical cord in order to allow nutrient transport, waste excretion and gas exchange between mother and fetus. The morphological features of the placenta differ among species, but the function is universal. The behaviour is characteristic to the mother of the majority of placental mammals. Significant documentation has been provided on placentophagy in a range of animals.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.
Ian Brockington is a British psychiatrist.
Postpartum blues, also known as baby blues and maternity blues, is a very common but self-limited condition that begins shortly after childbirth and can present with a variety of symptoms such as mood swings, irritability, and tearfulness. Mothers may experience negative mood symptoms mixed with intense periods of joy. Up to 85% of new mothers are affected by postpartum blues, with symptoms starting within a few days after childbirth and lasting up to two weeks in duration. Treatment is supportive, including ensuring adequate sleep and emotional support. If symptoms are severe enough to affect daily functioning or last longer than two weeks, the individual should be evaluated for related postpartum psychiatric conditions, such as postpartum depression and postpartum anxiety. It is unclear whether the condition can be prevented, however education and reassurance are important to help alleviate patient distress.
Psychoneuroendocrinology is the clinical study of hormone fluctuations and their relationship to human behavior. It may be viewed from the perspective of psychiatry, where in certain mood disorders, there are associated neuroendocrine or hormonal changes affecting the brain. It may also be viewed from the perspective of endocrinology, where certain endocrine disorders can be associated with negative health outcomes and psychiatric illness. Brain dysfunctions associated with the hypothalamus-pituitary-adrenal axis HPA axis can affect the endocrine system, which in turn can result in physiological and psychological symptoms. This complex blend of psychiatry, psychology, neurology, biochemistry, and endocrinology is needed to comprehensively understand and treat symptoms related to the brain, endocrine system (hormones), and psychological health..
Tokophobia is a significant fear of childbirth. It is a common reason why some women request an elective cesarean section. The fear often includes fear of injury to the baby, genital tract, or death. Treatment may occur via counselling.
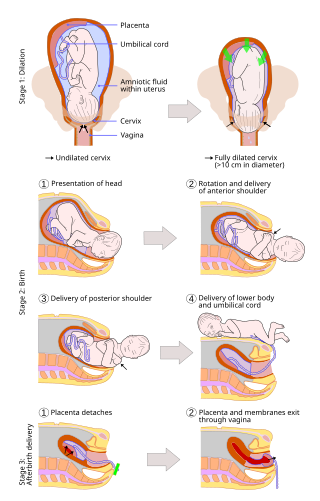
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than Caesarean sections (C-sections).

Postpartum psychosis(PPP), also known as puerperal psychosis or peripartum psychosis, involves the abrupt onset of psychotic symptoms shortly following childbirth, typically within two weeks of delivery but less than 4 weeks postpartum. PPP is a condition currently represented under "Brief Psychotic Disorder" in the Diagnostic and Statistical Manual of Mental Disorders, Volume V (DSM-V). Symptoms may include delusions, hallucinations, disorganized speech (e.g, incoherent speech), and/or abnormal motor behavior (e.g., catatonia). Other symptoms frequently associated with PPP include confusion, disorganized thought, severe difficulty sleeping, variations of mood disorders (including depression, agitation, mania, or a combination of the above), as well as cognitive features such as consciousness that comes and goes (waxing and waning) or disorientation.
A postpartum disorder or puerperal disorder is a disease or condition which presents primarily during the days and weeks after childbirth called the postpartum period. The postpartum period can be divided into three distinct stages: the initial or acute phase, 6–12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem. Long term health problems are reported by 31% of women.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
Childbirth-related post-traumatic stress disorder is a psychological disorder that can develop in women who have recently given birth. This disorder can also affect men or partners who have observed a difficult birth. Its symptoms are not distinct from post-traumatic stress disorder (PTSD). It may also be called post-traumatic stress disorder following childbirth (PTSD-FC)
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
Abuse during childbirth is generally defined as interactions or conditions deemed humiliating or undignified by local consensus and interactions or conditions experienced as or intended to be humiliating or undignifying. Bowser and Hill's 2010 landscape analysis defined seven categories of abusive or disrespectful care, including physical abuse, non-consented clinical care, non-confidential care, non-dignified care, discrimination, abandonment, and detention in health facilities.
Mental disorders can be a consequence of miscarriage or early pregnancy loss. Even though women can develop long-term psychiatric symptoms after a miscarriage, acknowledging the potential of mental illness is not usually considered. A mental illness can develop in women who have experienced one or more miscarriages after the event or even years later. Some data suggest that men and women can be affected up to 15 years after the loss. Though recognized as a public health problem, studies investigating the mental health status of women following miscarriage are still lacking. Posttraumatic stress disorder (PTSD) can develop in women who have experienced a miscarriage. Risks for developing PTSD after miscarriage include emotional pain, expressions of emotion, and low levels of social support. Even if relatively low levels of stress occur after the miscarriage, symptoms of PTSD including flashbacks, intrusive thoughts, dissociation and hyperarousal can later develop. Clinical depression also is associated with miscarriage. Past responses by clinicians have been to prescribe sedatives.