Related Research Articles

Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.
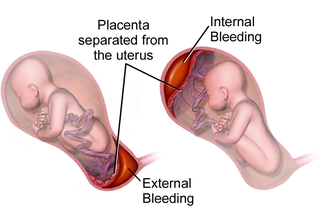
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.
Bloody show or show is the passage of a small amount of blood or blood-tinged mucus through the vagina near the end of pregnancy. It is caused by thinning and dilation of the cervix, leading to detachment of the cervical mucus plug that seals the cervix during pregnancy and tearing of small cervical blood vessels, and is one of the signs that labor may be imminent. The bloody show may be expelled from the vagina in pieces or altogether and often appears as a jelly-like piece of mucus stained with blood. Although the bloody show may be alarming at first, it is not a concern of patient health after 37 weeks gestation.

Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth. Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present. Disability or death of the mother or baby may result.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. The condition can occur up to six weeks following delivery.
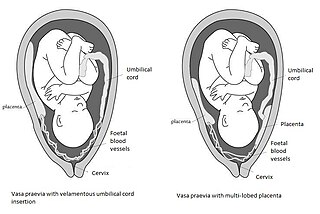
Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.
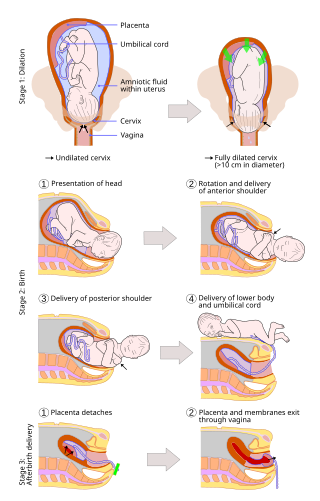
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than caesarean sections (C-sections).

Uterine inversion is when the uterus turns inside out, usually following childbirth. Symptoms include postpartum bleeding, abdominal pain, a mass in the vagina, and low blood pressure. Rarely inversion may occur not in association with pregnancy.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
A uterotonic, also known as an oxytocic or ecbolic, is a type of medication used to induce contraction or greater tonicity of the uterus. Uterotonics are used both to induce labor and to reduce postpartum hemorrhage.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.

Placental expulsion occurs when the placenta comes out of the birth canal after childbirth. The period from just after the baby is expelled until just after the placenta is expelled is called the third stage of labor.
Early pregnancy bleeding refers to vaginal bleeding before 14 weeks of gestational age. If the bleeding is significant, hemorrhagic shock may occur. Concern for shock is increased in those who have loss of consciousness, chest pain, shortness of breath, or shoulder pain.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.
References
- ↑ "ICD-11 for Mortality and Morbidity Statistics". World Health Organization. Retrieved 2023-12-05.
- 1 2 Vos, Theo; Allen, Christine; Arora, Megha; Barber, Ryan M.; Bhutta, Zulfiqar A.; Brown, Alexandria; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Z.; Coggeshall, Megan; Cornaby, Leslie; Dandona, Lalit; Dicker, Daniel J.; Dilegge, Tina; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Fleming, Tom; Forouzanfar, Mohammad H.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kawashima, Toana; et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577 . PMID 27733282.
- 1 2 Wang, Haidong; Naghavi, Mohsen; Allen, Christine; Barber, Ryan M.; Bhutta, Zulfiqar A.; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Zian; Coates, Matthew M.; Coggeshall, Megan; Dandona, Lalit; Dicker, Daniel J.; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Foreman, Kyle; Forouzanfar, Mohammad H.; Fraser, Maya S.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Huynh, Chantal; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kinfu, Yohannes; et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903 . PMID 27733281.
- 1 2 3 4 Walfish, M.; Neuman, A.; Wlody, D. (December 2009). "Maternal haemorrhage". British Journal of Anaesthesia. 103: i47–i56. doi: 10.1093/bja/aep303 . PMID 20007990.
- 1 2 Stables, Dorothy; Rankin, Jean (2010). Physiology in Childbearing: With Anatomy and Related Biosciences. Elsevier Health Sciences. p. 429. ISBN 978-0702044113.
- ↑ Say, Lale; Chou, Doris; Gemmill, Alison; Tunçalp, Özge; Moller, Ann-Beth; Daniels, Jane; Gülmezoglu, A Metin; Temmerman, Marleen; Alkema, Leontine (2014). "Global causes of maternal death: a WHO systematic analysis". The Lancet Global Health. 2 (6): e323–e333. doi: 10.1016/S2214-109X(14)70227-X . hdl: 1854/LU-5796925 . ISSN 2214-109X. PMID 25103301.
- 1 2 patient.info » PatientPlus » Antepartum Haemorrhage Last Updated: 5 May 2009
- ↑ The Royal Women’s Hospital > antepartum haemorrhage Archived 2010-01-08 at the Wayback Machine Retrieved on Jan 13, 2009
- ↑ Soyama H, Miyamoto M, Ishibashi H, Takano M, Sasa H, Furuya K (2016). "Relation between Birth Weight and Intraoperative Hemorrhage during Cesarean Section in Pregnancy with Placenta Previa". PLOS ONE. 11 (11): e0167332. Bibcode:2016PLoSO..1167332S. doi: 10.1371/journal.pone.0167332 . PMC 5130260 . PMID 27902772.
- ↑ Berghella, MD, Vincenzo (July 2017). "Cervical insufficiency". UpToDate.
- ↑ Charles J Lockwood, MD, MHCM, Karen Russo-Stieglitz, MD (July 2017). "Velamentous umbilical cord insertion and vasa previa". UpToDate.
- ↑ Atukunda EC, Mugyenyi GR, Obua C, Atuhumuza EB, Musinguzi N, Tornes YF, Agaba AG, Siedner MJ (2016). "Measuring Post-Partum Haemorrhage in Low-Resource Settings: The Diagnostic Validity of Weighed Blood Loss versus Quantitative Changes in Hemoglobin". PLOS ONE. 11 (4): e0152408. Bibcode:2016PLoSO..1152408A. doi: 10.1371/journal.pone.0152408 . PMC 4822885 . PMID 27050823.
- 1 2 Global burden of maternal haemorrhage in the year 2000 Carmen Dolea1, Carla AbouZahr2, Claudia Stein1 Evidence and Information for Policy (EIP), World Health Organization, Geneva, July 2003
- ↑ Kadir RA, Aledort LM (October 2000). "Obstetrical and gynaecological bleeding: a common presenting symptom". Clinical and Laboratory Haematology. 22 (Suppl 1): 12–6, discussion 30–2. doi:10.1046/j.1365-2257.2000.00007.x. PMID 11251653.
- ↑ Aldred, Heather E. (1997). Pregnancy and birth sourcebook. health reference series. ISBN 9780780802162.
- 1 2 3 4 5 6 Heine PR, Swamy GK (August 2009). "Vaginal bleeding during early pregnancy". Merck Manual.
- ↑ Aldred, Heather E. (1997). Pregnancy and birth sourcebook. Omnigraphics. ISBN 9780780802162.